Health and wellbeing boards up and down the country are leading local efforts to reduce premature mortality, helping people and communities move towards better health and reducing demand on hard-pressed local authority and health resources.
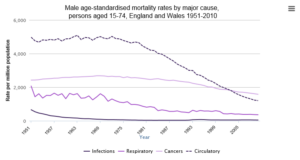
Tackling the epidemic of chronic diseases – or non-communicable diseases (NCDs) – is at the heart of this agenda, and it’s a major challenge. First, we have to speed up the fall in death rates from major NCDs. The graph below shows the declines across respiratory, cancer and circulatory diseases. The trends are encouraging, but we need to do better: the Global Burden of Disease – the international study that quantified the loss of health due to diseases and risk factors – found that the UK lagged behind many other western industrialised countries in reducing premature mortality rates.
And the disease burden is not spread evenly across the population. For instance the premature mortality rate from heart disease and stroke in Manchester is 2.5 times higher than that of Dorset, and the premature mortality rate from lung disease in Blackpool is 4 times that of Suffolk.
Another problem is that, while life expectancy has risen, for too many people, a longer life involves more years spent with chronic disability. The Global Burden of Disease also highlighted the toll taken by musculoskeletal (such as low back pain) and mental disorders in particular. Then there’s the sheer numbers of people affected: over 15 million, or roughly a quarter of the population, has a long-term condition (which includes major NCDs) and the number of people with multiple conditions is expected to rise, presenting a challenge to health and social care.
Furthermore, the prevalence of most of the major NCDs is on the rise, partly because of better detection but also because of “genuine” rises – driven in part by an ageing population.
Another issue we face is the evolving nature of the risk factors for NCDs. Tobacco (from smoking and other sources) remains the leading risk factor, accounting for the largest share of disease burden in the UK, followed by high blood pressure and being overweight. Others include a poor diet, insufficient physical activity and alcohol use. And while we’re seeing positive trends in some areas (e.g. declining smoking rates and the reduction in salt intake across the population), we’ve had less success elsewhere.
These risk factors don’t exist in isolation. As local authorities are all too aware, they are shaped by the contexts of people’s lives - their homes, workplace, schools and wider communities – and are influenced by social and structural factors, including socio-economic status and social exclusion. This means that an effective strategy for NCDs requires concerted action on these behavioural risk factors, as well as on the many underlying influences that drive them (such as housing, employment, transport, income and environment). It’s by tackling these deep-seated “causes of the causes” that we can start to address the inequalities in health and lay the foundations for health earlier on in people’s lives. Local authorities, through their public health teams and health and wellbeing boards, will lead the local efforts on this.
This is a direction of travel that is widely advocated: internationally, the focus is on the need to create health-promoting environments, as well as taking specific actions on known risk factors.
In our country, the Secretary of State for Health has highlighted this opportunity in his call to action: Living Well for Longer , which challenged the health and care system to improve England’s rates of premature mortality. Such strategies acknowledge that NCDs are complex problems, which require coordinated and sustained action, at a local level and at scale.
So what is PHE’s vision for how we can support local areas to move the entire population towards better health and wellbeing, while intensifying our efforts for those individuals and communities in greatest need?
A good place to start is by recognising and capitalising on the amazing assets we have across the health and care system, at both local and national levels, for preventing and intervening early on NCDs.
Local authorities now have a duty to improve the health of local communities. They commission a range of prescribed NCD services, including NHS Health Check and the National Child Measurement Programme. Local health and wellbeing boards develop and respond to their public health priorities – which could be tackling obesity, for example, or drugs and alcohol misuse. This new duty sits alongside local authorities’ other responsibilities to address the wider determinants of health, including jobs, housing, environment and transport – a great opportunity for concerted local action.
NHS England is responsible for providing high quality treatment and care, as well as commissioning key NCD public health services, including cancer and non-cancer screening services, children’s public health services for 0-5 year olds (until 2015), immunisation and public health services for those in detention settings.
Clinical Commissioning Groups are responsible for designing local health services in England, working with patients and healthcare professionals, in partnership with local communities and local authorities. They commission health and care services.
An effective fight against NCDs will require the collaboration of all of these organisations, as well as the partnership of many other stakeholders – including local communities, the voluntary and community sector, business and sectors from housing to transport.
In this new environment, PHE’s role is to support local action by providing specialist advice, data and tools. These can help to translate evidence into action, and share best practice. PHE also brings together programmes and expertise that - working in partnership with our 15 PHE Centres - can support our local partners in their health improvement efforts.
But our ambitions don’t stop there. Below are three areas where I believe PHE can and should aim to accelerate our efforts to tackle NCDs.
We need to engage the public in new ways about their health and wellbeing. There’s an important national debate to be had about how health and wellbeing is created and sustained. Most of us want to live as long, as well, and as healthily, as we can. The reasons we sometimes don’t are complex. We may lack, or feel we lack, a sense of control over our lives, face obstacles (like living in an unsafe neighbourhood, or coping with a mental health problem), or think a healthy lifestyle is less of a priority than finding a job or a home.
But the scale of the NCD challenge means that we need an engaged and health- literate population; one that understands the opportunities for improving health; and can access the tools to create and maintain health across the lifecourse. The internet and social media can be empowering in this context and public health needs to embrace this personalized approach.
PHE is committed to supporting a new national conversation on health and wellbeing. We’ll do this through our work in raising the profile of prevention and early intervention, and through making our programmes as relevant as possible to people and communities, in terms of what matters to them.
We must continue to develop and implement effective, high-quality, acceptable, affordable and scalable programmes, which drive health impact and reduce inequalities.
The work of our academic colleagues and the National Institute for Health and Care Excellence now gives us a better understanding of what works in preventing and controlling NCDs. However, we need to do better at prioritising the right interventions for the right populations, implementing them effectively, and scaling our efforts to maximise health impact. This is especially important during tough economic times when effectiveness, cost-effectiveness and return on investment considerations are key.
PHE contributes to this effort by providing expert advice and support to local government and the NHS on: public health issues (smoking, alcohol, drugs, mental health, physical activity, blood pressure control, diet and obesity, sexual health); health marketing and behavioural change; health equity (healthy places, sustainability); and prevention programmes (NHS Health Check, screening).
We work to promote health and wellbeing throughout the lifecourse, with teams focused on Children, Young People and Families, Healthy Adults and Healthy Older Adults. We are also committed to tackling the conditions that account for major disability, including mental health disorders and musculoskeletal conditions, which often receive too little emphasis.
Our health improvement programmes are supported by world-leading knowledge and intelligence systems. These provide relevant and timely information to local and national decision makers, on the most important indicators. Assets such as the Public Health Outcomes Framework and Longer Lives, can highlight variations, and allow us to monitor and evaluate progress.
Data can also help us to fight NCDs more effectively by identifying which areas offer the greatest scope for improvement. For example, targeting hitherto neglected areas, such as hypertension, could yield big improvements in preventable mortality.
Finally, we need to create a “culture for health” that is knitted into the fabric of our day-to-day routines.
Given our understanding of the social, economic, environmental and commercial determinants of health, it is critical that tackling NCDs is not seen solely as the responsibility of the health sector, but engages a coalition of sectors and partners, at national and local levels. Prevention is more impactful and sustainable when it is embedded both within health services and across wider society.
Smoking restrictions in public places, reducing salt in food manufacturing as well as dietary intake of saturated fat and sugar, alcohol pricing, insulating homes, safe and active travel routes to school: these are just some examples of ways we can change the environment to promote health, for the long term and across the lifecourse.
Different parts of the system each have key roles to play in making this happen. The Department of Health and other government departments will continue to define the national ambition, set national priorities, allocate resources throughout the system, promote cross-Government action, broker partnerships (such as the Public Health Responsibility Deal) and, when necessary, introduce legislation.
Local governments clearly also have a critical role in setting local policies and ambitions, in integrating health into social and environmental approaches, and championing the health and wellbeing of their communities.
PHE will play its part in providing the data, intelligence and knowledge to enhance strategic planning, inform prioritisation and decision-making, share promising practices, and monitor and evaluate results.
The scale of the NCD epidemic is such – in its cost to society and the burden on individuals and families – that we need to do things differently. We need an approach that combines the power of population level strategies, with the commitment to improve local environments, and the strategies to shift individual behaviours, so that it’s easier to be healthy. I am confident that working together, we will help to make a difference in all of these areas.

1 comment
Comment by Bren posted on
Hello Kevin,
A complex picture taken down to succinct and famed messages for us all.
I think the timing of the contributions that individuals in communities can give is a crucial one and above all it is about trust and relationships. Trust and relationships being such a powerful part of the environment in which the actions happen.
I think they key component that is needed,and needed to be maintained is the environment, it being safe, welcoming, open, honest an above all has a mutual understanding of one another.
It is a journey, and a journey that has junction points but is not an end.
Thanks and keep well and all good wishes,
Bren.