
Recently we announced figures detailing the level of uptake of the NHS Health Check programme across the UK, which show that in the last year, 1.4 million eligible people have accepted the offer, an increase on the previous year by 7.4%.
The NHS Health Check was introduced in April 2009. It is a universal risk assessment and risk management programme offered every five years to people aged 40–74, who have not previously been diagnosed with vascular disease.
The programme is part of a long overdue approach to engage and activate the public about their health, focus on prevention and risk reduction, and strengthen place-based leadership for health improvement.
England currently faces a burden of non-communicable diseases, such as heart disease, certain cancers, type 2 diabetes and liver disease, all of which are largely preventable.
Around two-thirds of deaths among people under the age of 75 in England are estimated to be avoidable, and there are still high numbers of undiagnosed cases of preventable disease.
For instance, there is currently an estimated minimum of five million undiagnosed cases of hypertension, 750, 000 undiagnosed cases of chronic kidney disease (Stages 3–5) and 500,000 undiagnosed cases of type 2 diabetes in England.
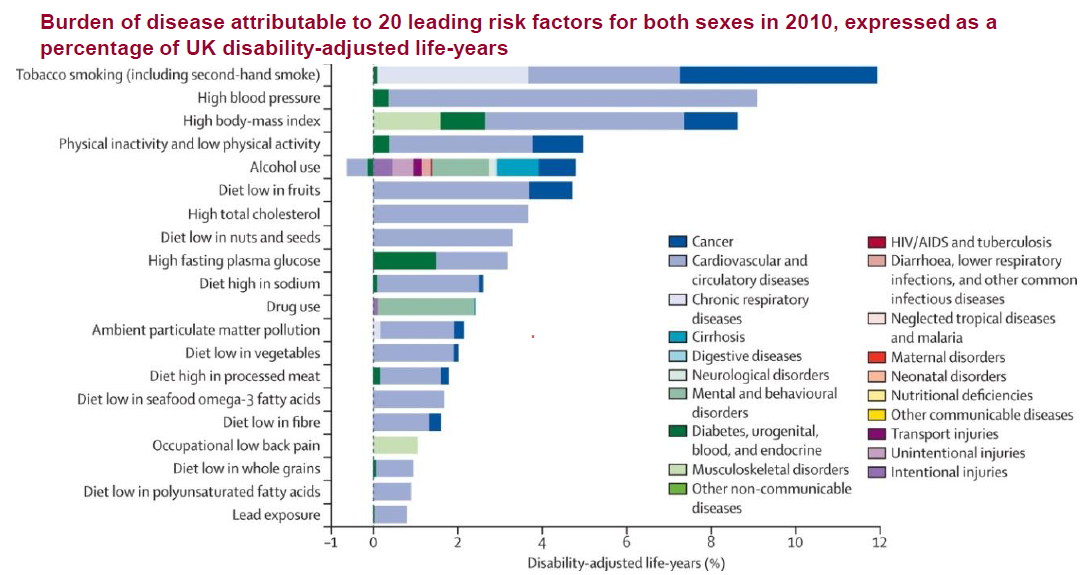
To combat this epidemic, we introduced the NHS Health Check as part of a larger scale action plan to focus on the top seven behavioural and physiological risk factors that drive preventable mortality and morbidity: smoking, hypertension, obesity, physical inactivity, alcohol, poor diet and high cholesterol.
Tackling these risk factors remains in line with the aims of the recently published NHS Five Year Forward View and Public Health England priorities, which argue for a ‘radical upgrade’ in prevention.
 We are committed to achieving the best possible outcomes from the NHS Health Check by optimising the programme from beginning to end. To do this, PHE has set out an action plan to address improvements around the governance of the programme and ultimately drive increased uptake of the service.
We are committed to achieving the best possible outcomes from the NHS Health Check by optimising the programme from beginning to end. To do this, PHE has set out an action plan to address improvements around the governance of the programme and ultimately drive increased uptake of the service.
As around a fifth of the population will be invited each year to participate in the programme, we are ambitious in our aim for future take up of the service.
We have been achieving around 50% uptake in the first few years, which is promising, and we are continuing to support work that encourages people to take up this important check.
While PHE remains responsible for the national coordination and leadership of the programme, we are also supporting local authorities, who have been responsible for commissioning of the programme since 1 April 2013.
We’ve developed new tools and resources to aid local authorities with implementation, including a marketing toolkit and directory, information governance and data flow tool, a set of programme standards as well as best practice guidance.
It is key that we continue to offer this support, as many local authorities not only now consider NHS Health Check as a core offering within their adult health improvement programmes, but are also driving innovation around how the programme is delivered.
For instance, in some areas, local authorities take a targeted approach prioritising local communities at with the greatest health risks
In addition, local authorities have been expanding the range of providers offering an NHS Health Check, including pharmacies, major retailers and voluntary sector agencies, thereby potentially broadening access to the programme beyond GP surgeries.
Indeed, NHS Health Check provides local government and the NHS with an opportunity to consider new ways of embedding public health across their communities.
A programme of this scale has never been done before and being a world leading initiative, we are committed to evaluating its clinical and cost effectiveness.
We are also aware that a number of concerns have been raised about the programme. These generally fall into three broad categories: the evidence for the effectiveness of the programme; the implications for population-level approaches; and the potential impact on health inequalities.
As with any large-scale prevention programme, we acknowledge that there are some risks inherent in delivering the NHS Health Check. We are currently awaiting the publication of two national evaluations to provide an early assessment of outcomes since implementation began.
This evaluation will form part of our commitment to bring greater scientific rigour to the programme alongside our work to establish the Expert Scientific and Clinical Advisory Panel (ESCAP), content review process and the priorities for research.
We welcome constructive debate and view it as important to help spur the on-going development and improvement of our prevention programmes, including NHS Health Check.
The programme gives us an opportunity to address the growing rate of preventable illness in the country and the high levels of undiagnosed and untreated chronic diseases. These are not only devastating for those affected but are also a huge burden on the NHS and social care services.
We are assessing and building upon the early implementation lessons to improve programme delivery to ensure that the NHS Health Check supports and enhances local health improvement. Our efforts are now focused on ensuring that NHS Health Check promotes population-wide health gain; is fully integrated with other local health improvement programmes, and is getting the best value and health impact for the investment through improved programme management, better implementation, robust evaluation and appropriate targeting.
To find out more about the progress of the NHS Health Check, read PHE’s latest article in the Journal of Public Health.

2 comments
Comment by Bren posted on
Hello Jamie,
A great blog and thank you.
I too have come across the challenges to the Health Check programme and I am sure the plan in place will address these. I am also sure the two national evaluation reports will be useful too in going forward.
Maybe look at the community sector too in your planned work, and make links with people who are close the people PHE is looking, particularly to reach. May be use the PHE People's Panel for support in this area too.
A great blog and thank you,
Bren.
Comment by Cara Lane posted on
How does PHE know the data LAs are submitting is accurate? Is the data verified? Eg. If LAs claim they are sending invites over a 5 year period to 100% of the eligible population, but uptake is nowhere near that figure (so say 50% or less), how does PHE know the LAs, and the LAs know the GPs and other providers, are not just making up the data about numbers of invites sent? There are only 2 eligible adults in my family of 3 (the 3rd being school age!). Here we are 4 years out of 5 into the programme and neither adult has been invited! What's the betting that my LA will claim at the end of the 5 year period that they've invited 100% of the eligible population (they are at 85.5% offers already, but uptake is only at 39%) and myself and my husband will still not have been invited or have received an NHS Health Check? Caution PHE!