Last week Cancer Research UK released a press release showing that bowel cancer is more likely to be diagnosed at the earliest stage if it is picked up by screening. This used new PHE data that, for the first time, shows the stage (one to four) at which cancer is detected by the different routes to diagnosis – like screening, GP referral or as an emergency.
To get this data we looked in detail at people diagnosed in 2012 and 2013 and examined the stage of their cancers at diagnosis.
This new analysis has given us brand new insights into the diagnosis of over half a million patients diagnosed with cancer, for example:
- more early stage ovarian cancers present through GP referral and other managed routes, compared to the Two Week Wait (urgent GP referral with a suspicion of cancer) route
- many uterine cancers in older women (over 80 years old) are picked up at an early stage, when the cancer is still treatable
- more early stage melanomas in females present through the Two Week Wait route, compared to males
- late stage lung cancers present through all routes, not just as emergency presentations
Stage at diagnosis strongly predicts cancer survival, and for some cancers (including lung and colorectal), UK patients are diagnosed at a later stage than those in other comparable countries. It is important that we understand more about the patients diagnosed at different stages, so that we can better inform what needs to be done to improve survival and other patient outcomes.
In November 2015 we published new results from the Routes to Diagnosis study (read the accompanying blog “Big data in action: The story behind Routes to Diagnosis”). In that we used the latest available data to produce an extensive set of results for over 2 million patients diagnosed with cancer between 2006 and 2013.
The new study, undertaken in partnership with Cancer Research UK, adds staging information for 10 cancer types diagnosed in 2012 and 2013, to assess the variation in stage distribution by Route.
Data by stage for bladder, breast, colorectal, kidney, lung, melanoma, non-Hodgkin lymphoma, ovarian, prostate and uterine cancers are stratified by sex, age, socio-economic deprivation quintile and ethnicity.
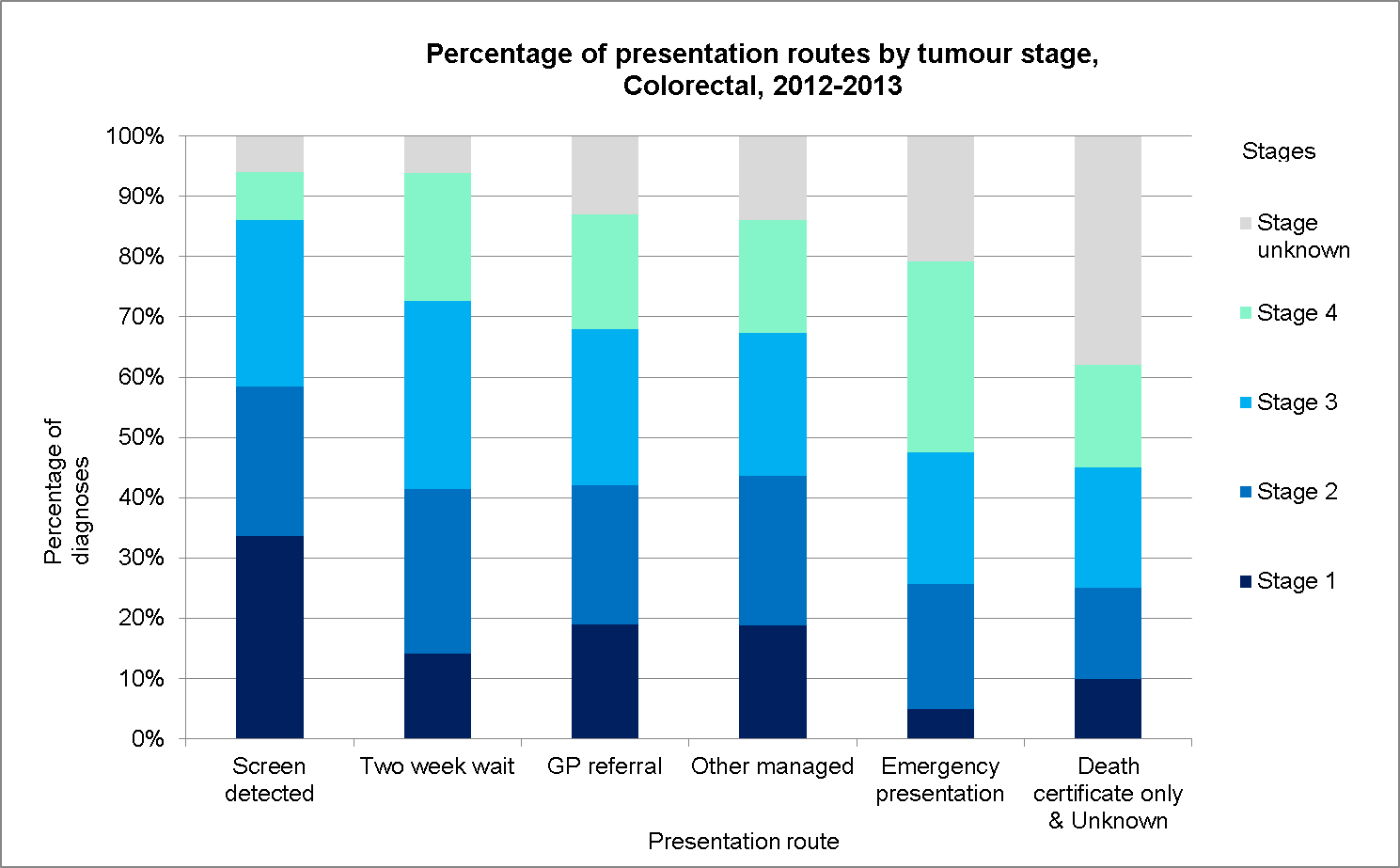
Six route groupings are presented: screen detected, Two Week Wait, GP referral, other managed pathways (which combines inpatient elective and other outpatient), emergency presentation and a category combining death certificate only and unknown route.
An Excel workbook is available to download which contains all of the results along with graphical displays, for example for colorectal cancer:
Talking to cancer staging experts, these results are not unexpected, although they have not been presented on this scale before. So do these results give us any new answers, or do they only pose further questions? What might be the reasons behind the results that we see?
For some cancers (e.g. lung and ovarian) the majority of emergency presentations are at an advanced stage, whereas in other cancers (e.g. bladder and uterine) the emergency presentations are made up of people in all stage groups.
It is likely that biological differences and the ‘symptom signature’ of various cancers play some part here. However, this also means that a minority of patients with early stage cancers are diagnosed though emergency presentation. This finding is intriguing: are these emergency presenters with early stage disease emergency GP referrals (and if so, what are the circumstances leading to them?), or A&E self-referrals for symptoms for which other patients would first consult with their GP? We would need to link our data to other datasets to investigate this further.
When we look at Two Week Wait (TWW) compared to other GP routes, we also see differences between cancers. For a patient to be referred by their GP as a TWW, they need to display certain symptoms as defined in guidance from the National Institute for Health and Clinical Excellence (NICE), often referred to as red-flag symptoms. Our results show that for some cancers these red flags are associated with more advanced stage (e.g. colorectal and lung), whilst the opposite is true for other cancers (e.g. uterine and melanoma).
The NICE guidelines were revised this year, with many referral thresholds lowered: will future results show more people being referred though this route at an earlier stage?
Our results also highlight differences by age, sex, deprivation and ethnicity. We hope that by making these data available for all to use and examine, we are adding to the knowledge that helps to make improvements in diagnosing cancer earlier.