The role of healthcare providers is to investigate, treat and care for people who are ill, but they also have huge potential to act as public health organisations at a time when prevention and early intervention have a crucial role to play.
Recently I met with the Provider Public Health Network– a group of public health professionals who work in or closely with hospital, community or mental health trusts in England. It was a great opportunity to learn more about their experience of working in trusts and discuss the challenges and opportunities this presents for public health.
A wide range of public health activity takes place in NHS trusts – from setting up alcohol screening programmes to running sexual health services and developing trust-wide public health strategies.
Indeed, public health skills can be applied across almost all trust business, including health improvement activity with patients, staff and the public, the development and delivery of health services for communities and a number of health protection functions such as infection control and immunisation.
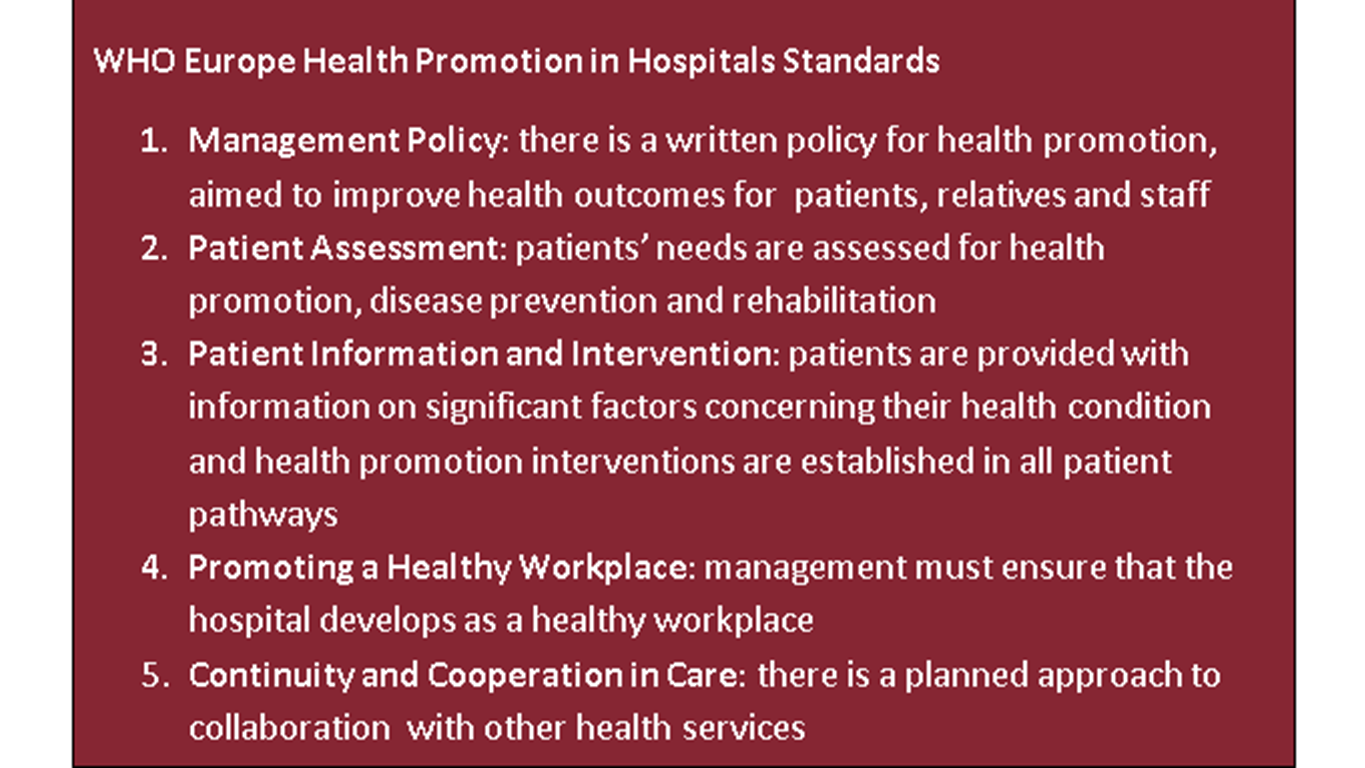
More than a decade ago, the World Health Organization initiated the Health Promoting Hospitals (HPH) movement to support hospitals to place more emphasis on health promotion and disease prevention rather than on diagnosis and curative services alone. A number of trusts across England use the HPH framework standards (see below).
Prevention is key
We are all aware of the pressures currently facing healthcare providers, yet it is now timely to revisit their role as public health organisations. NHS budgets are strained and the burden of preventable diseases continues to rise; 1 in 7 NHS hospital beds are occupied by people with diabetes, while every year, 1 million hospital admissions are related to alcohol use. If we are to sustain our health service into the future, trusts must place more emphasis on, and investment in, prevention and early intervention activity.
The NHS Five Year Forward View set out a compelling vision for the NHS, much of which requires a public health and population-based approach to help us implement it, such as hard-hitting action on obesity, smoking, alcohol and other health risks, and the roll-out of a national diabetes prevention programme.
A number of elements of this strategy are particularly relevant now:
- Trusts need to ensure that the care they provide is high value, effective and cost-effective.
- Growing levels of obesity, alongside continuing impact of alcohol use and smoking, is increasing demand for healthcare.
- Healthcare providers have the potential to improve the health of every person who comes through their doors through initiatives such as Making Every Contact Count.
- A trust’s biggest asset is its staff, and the health and wellbeing of its workforce (2 million staff within acute and community Trusts alone) is fundamental to maintaining their capacity and capability to provide high quality services.
- Trusts can play a significant role in their community, as big local employers and procurers of goods and services.
So how can we support and develop provider public health roles in order to help trusts improve population health in the face of current pressures on resource?
Sharing experiences
There are some great examples of how public health expertise has contributed to trusts’ core business and requirements including leading initiatives on alcohol, smoking cessation and tackling domestic violence, advising on action required based on interpretation of data and evidence and working with clinicians to improve service quality and outcomes.
For example, Blackpool Teaching Hospitals Foundation Trust has set up an inpatient tobacco specialist service, managed within its public health team. An education practitioner trains staff and volunteers to identify tobacco users and give brief advice on smoking, while two tobacco liaison specialists offer ‘bedside’ support, ensure patients have access to NRT and lay the foundations for quitting long term. Once patients are discharged, they are referred on to the stop smoking service in the community, to ensure continuity of care. Some volunteers have received additional training to support pregnant women and new parents in the women’s and children’s unit. The service exceeds its key performance indicators each month, set by Blackpool council to include the number of smokers referred to stop smoking services and compliance with the hospital’s smoke free policy.
I also heard about the challenges: health improvement is often not included in training for clinicians and is not yet part of the culture of many providers, who are faced with competing targets and financial priorities.
Yet healthcare providers have huge potential as public health organisations to improve public health and healthcare, and public health expertise can add real value to their core business. In order to maximise this potential, trusts must buy into and own public health activity, supported by those at a senior level. In order to get that buy in, we must find ways to define outcomes and measure impact to demonstrate to trusts the value of public health approaches.
Targets to incentivise public health activity can help trusts to measure the impact of their investment, while dedicated public health staff, including at director level, will also help to drive this forward.
The Provider Public Health Network is an independent group with a membership of more than 60 Public Health professionals who work in or closely with provider trusts. For more information contact mandy.harling@phe.gov.uk or janecwells@yahoo.co.uk (network chair).


1 comment
Comment by Dr Nasiruddin posted on
All relevant at this stage- but my concern arises when PHE clashes with primary care in targeted deprivation agendas. Primary care should be universal access for all and most health inequalities are socially driven ( as per the Black report- pushing medical management here doesn't effect change) and I don't think it's an effective highjacking of primary care finding. Furthermore increased " local" agendas ignore variations between local practices which can be enormous- disincentivises individualisation and best practice in surgeries as pushes dumbing down to lowest common denominator in practice under the guise of "equality"!