Welcome to the latest edition of PHE’s Health Matters, a resource for local authorities and health professionals, which for this edition focuses on the decline in cervical screening attendance in England and outlines what can be done to boost screening coverage.
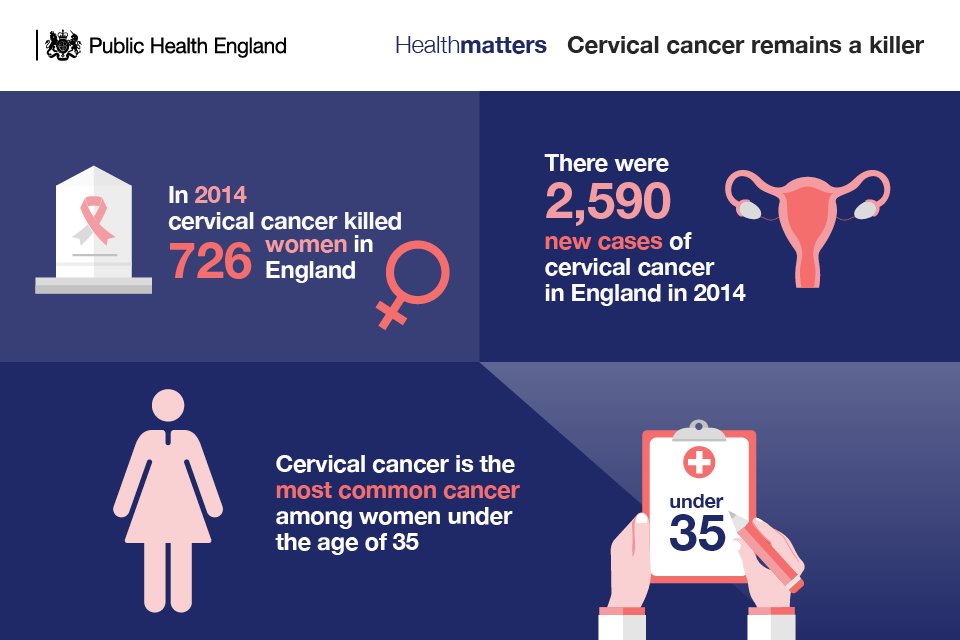
Although cervical cancer mortality rates have decreased by up to 70 per cent since the introduction of the NHS Cervical Screening Programme in 1988, there were still 726 deaths from the disease in England in 2014 and a total of 890 in the whole of the UK.
Worryingly, screening coverage has fallen over the last 10 years and attendance is now at a 19-year low. Coverage is going down across all age groups.
Screening figures collected by NHS Digital show that coverage amongst women aged 25 to 49 years was 70.2% at 31 March 2016. This compares to 71.2% as at 31 March 2015 and 73.7% as at 31 March 2011.
For women aged 50 to 64 years, the coverage at 31 March 2016 was 78.0% which compares to 78.4% as at 31 March 2015 and 80.1% as at 31 March 2011.
At a regional level, coverage of the full eligible age group in 2016 ranged from 66.7% in London to 75.9% in the East Midlands. The vast majority of reporting regions reported a fall in coverage at 31 March 2016 when compared with 2015.
51 out of 160 local authorities achieved coverage of 75% and above. 58 local authorities achieved coverage of 70% to less than 75%. The national target for cervical screening coverage is 80%.

Women are offered screening every 3 or 5 years depending on their age. Women aged 25 to 49 are invited for routine screening every 3 years, whereas those aged 50 to 64 are invited for routine screening every 5 years.
Cervical screening is not a test for cervical cancer. Screening is intended to detect abnormalities within the cervix that could, if undetected and untreated, develop into cervical cancer.
It is estimated by UK researchers that in England cervical screening currently prevents 70% of cervical cancer deaths. However, if everyone attended screening regularly, 83% could be prevented.
However, a number of barriers exist that are hindering women from attending. The most common reasons for not attending screening are embarrassment about having a smear test and worry about the outcome of the test.
Several studies have identified groups that are frequent non-attenders for screening which includes women over 50, younger eligible women, women from ethnic minority groups, as well as lesbian and bisexual women.
What can you do?
This edition of Health Matters outlines how local authorities, Clinical Commissioning Groups (CCGs), and GPs can all play a key role in raising awareness of cervical screening and encouraging women to attend screening.
Although screening is most commonly delivered in primary care, local authorities have a crucial role to play in raising awareness of cervical screening. Local authorities can work directly with GP surgeries to raise awareness of screening as well as through outreach work with women in their communities.
GPs and practice nurses can play a central role in educating women and therefore in increasing attendance for screening.
All women must be given the opportunity to make an informed choice about whether or not to attend for cervical screening. The decision should be based on an understanding of:
- why they are being offered screening
- what happens during the test
- the benefits and risks of screening
- the potential outcomes (including types of result, further tests and treatment)
- what happens to their screening records
Read more about ways to make cervical screening more accessible in this edition of Health Matters which includes a set of infographics and slides to support local commissioning and service delivery, as well as best practice case studies.
Visit the Health Matters area of GOV.UK to see the wide range of topics Health Matters has covered (other recent editions have looked at child dental health and obesity/food environment) or sign up to receive the latest updates through our e-bulletin.
And if you found this blog helpful, please view other Health Matters blogs.
Health Matters
Health Matters is a resource for professionals which brings together the latest data and evidence, makes the case for effective public health interventions and highlights tools and resources that can facilitate local or national action. Visit the Health Matters area of GOV.UK or sign up to receive the latest updates through our e-bulletin. If you found this blog helpful, please view other Health Matters blogs.

7 comments
Comment by katrehman posted on
May I make a suggestion? Personally I'm not convinced awareness needs to be raised any more about smear testing. Women receive "invitations " reminders and more letters,their records are flagged if they are "overdue " and it's brought up in the next time they attend the surgery even if all they want to discuss is their bunions. ..you are offering a service to women and they're not taking it up. Instead of yet another awareness campaign why not use the money to send questionnaires to women asking what they want from the programme? If uptake is falling maybe women are making an informed decision not to test. As we are told it's our choice why then the surprise not all choose to have the test? They could be sourcing a self test kit for HPV privately? There are all sorts of reasons they don't go. I think it's just convenient to blame embarrassment. And if some are embarrassed why not look at offering a more acceptable alternative?
Comment by Nicola Patterson posted on
Accessible is the key word here. I would think the vast majority of smears are taken in GP surgeries by Practice Nurses. Maybe we should have more alternative places available to have the test. Busy women, especially those working and trying to find time out of work,home, childcare etc, find it hard to go to their GP surgery during a full busy week. For a lot of women, going to a sexual health clinic for their routine smear is not attractive. How about pharmacies in the bigger stores (in a private room of course!) with trained nurses. Not everything has to be done at a GP surgery! I am a Practice Nurse myself and recently got my invitation for a smear. I found it extremely difficult finding time to book in at my GP surgery and thought how easy it must be for people not to bother when it is so difficult to get a convenient appointment
Comment by Deirdre posted on
I have just read an article that menstrual blood can be used to detect the presence of HPV. So why not give women the chance to send in a sample? This would save every body much time and money. Self-testing kits are also available as part of the Dutch cervical screening programme. Why not here? Women have a choice and are now realising that without HPV they cannot get this cancer. Isn't it time that truthful information about this cancer was made publicly available, and the scolding and patronising attitudes which treat women like naughty schoolgirls were stopped?
Comment by Kiwicelt posted on
I would suggest that many women are now doing their own research and making informed decisions to decline this screening. Why is that so hard to understand? There are many women who have been coerced into this screening over the years without any informed consent who are now getting actual, factual information. No one ever mentioned that there were harms associated with cervical screening or that the rates of overtreatment are horrendous. There was also never any mention of the potential for increased rates of C section or premature rupture of membranes in pregnancy with the LLETZ procedure. Many young women submitted to cone biopsy and other such butchery of the cervix, particularly in the early days of the NHS screening programme.If PHE were serious about giving choice about screening they would remove the screening targets and measure the success of the programme by the number of women who are actually making informed choices. It should be accepted that an informed decision to decline screening is just as valid a choice as the decision to attend.
Comment by Kate posted on
I strongly agree that women are making an informed choice to not have the test. It is not about not knowing the test exists, it is because the test is so unpleasant. I refuse to have it. A smear test feels like a sexual assault to me (speculums were designed for use on slave women in the United States and have never been redesigned) and it will be an extremely cold day in hell before I have another one.
Comment by Jenny Greenfield posted on
Its interesting that since Public Health England decided to do away with nurse consultants with a remit for increasing the uptake of cervical screening that targets have decreased even more. It is necessary to have dedicated professionals working together to promote screening.
Comment by ARC posted on
I echo the comments of others that it is highly inconvenient for women to make this appointment to go into their GP surgery and screening needs to be available in more places and perhaps at weekends. It would be much easier to make an appointment on a Saturday for a screening service near a shopping or leisure centre for the many women who work and look after children during the week. I remember that I used to be able to make an appointment for screening at anytime but now I have to come during certain days of my cycle and with irregular cycles, it is difficult for me to calculate in advance when that will be.