Welcome to the latest edition of PHE’s Health Matters, a resource for local authorities and health professionals, which for this edition focuses on preventing infections and reducing antimicrobial resistance (AMR).
Preventing infections from occurring in the first place is one of the best ways to prevent AMR. Antimicrobial resistance can be developed in bacteria, viruses, fungi and parasites that cause infection, making them resistant to treatment. Every infection prevented reduces the need for and use of antimicrobials, which in turn lessens the potential for development of resistance.
Antibiotics are by far the most widely prescribed antimicrobial agent. Unlike many other drugs used in medicine, the more we use antibiotics the less effective they become against their target organisms. With antibiotics, overuse or inappropriate use allows bacteria to develop resistance which can lead to infections that are increasingly difficult to treat.
A failure to address the challenge of antimicrobial resistance could result in:
- An estimated 10 million deaths every year globally by 2050.
- A cost of £66 trillion in lost productivity to the global economy.
Currently in the UK, the greatest and increasing threat from drug resistant organisms is from Gram-negative bacteria. Gram-negative organisms normally live in healthy individuals but can also cause significant illness and death in some instances. They can cause focal infections in many organ systems but are particularly dangerous when they infect the blood and cause sepsis, a potentially catastrophic systemic infection.
Infections caused by Gram-negative organisms are increasing. This latest edition of Health Matters focuses on what can be done to prevent infections, with a focus on Escherichia coli bacteraemia (E. coli) which accounts for 55% of all Gram-negative BSIs.
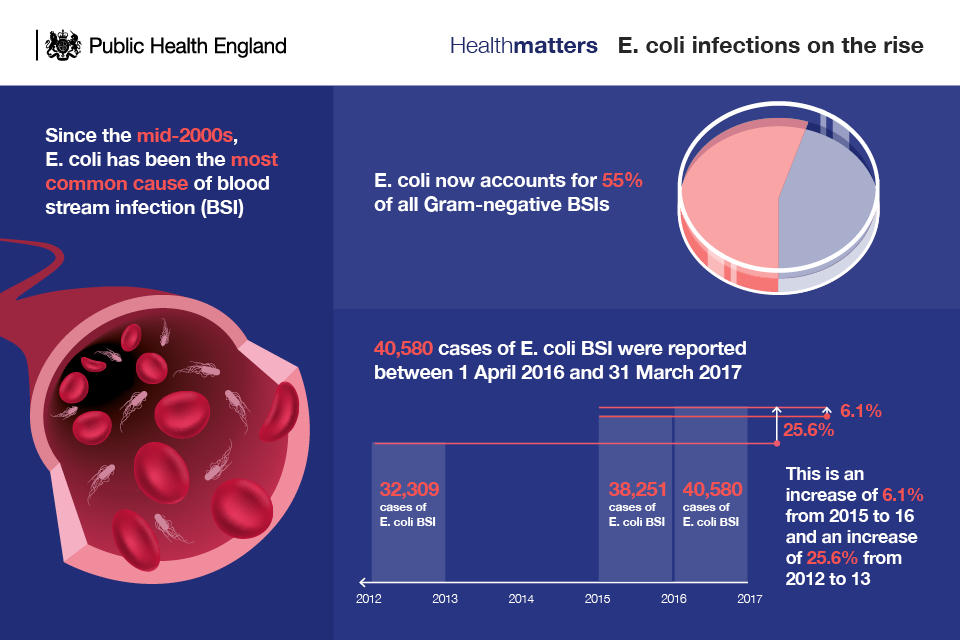
Over 40,000 cases of E. coli BSIs were reported by NHS trusts in England between April 2016 and March 2017, an increase of 6.1% from 2015-16 and an increase of 25.6% from 2012-13.
The government has acknowledged the need for action and has set an ambition to reduce healthcare associated Gram-negative BSIs by 50% by 2021 and reduce inappropriate antimicrobial prescribing by 50% by 2021.
Comprehensive infection prevention and control (IPC) measures are the cornerstone of any approach to reduce the development and spread of infections including antimicrobial-resistant infections
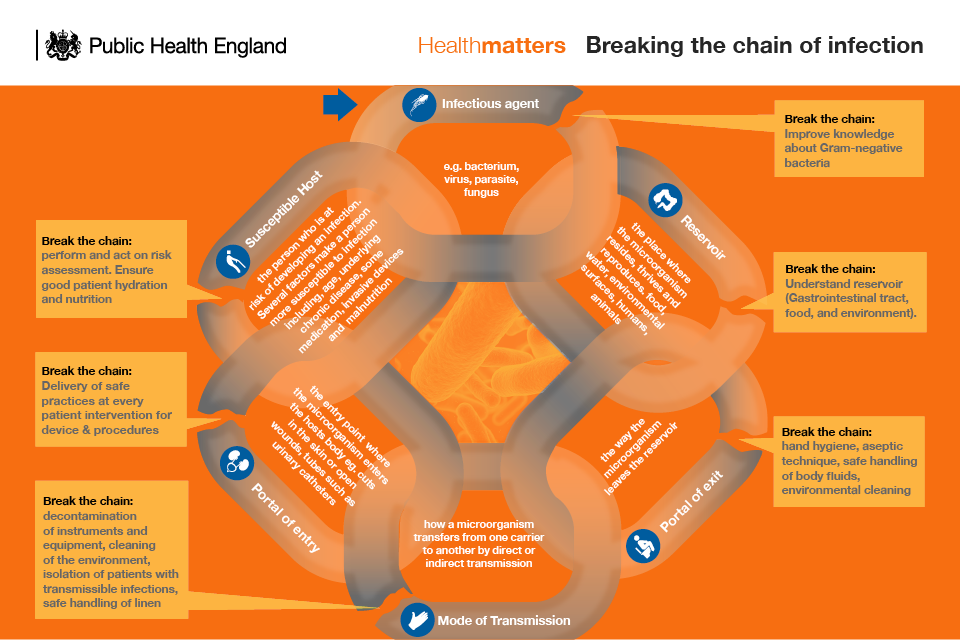
This edition of Health Matters will use the Chain of Infection model to illustrate how the actions of health and social care workers play an essential role in breaking the chain and preventing the spread of infections such as E. coli. For widespread improvement and to realise our ambitions we must move to a whole health system approach that spans health sector boundaries and looks at the whole patient pathway.
Read this edition of Health Matters to find out how healthcare professionals across primary and secondary care, community care professionals, specialist IPC teams, and senior leadership can all contribute towards preventing infections. It includes a set of infographics and slides to support local commissioning and service delivery, as well as best practice case studies.
Visit the Health Matters area of GOV.UK to see the wide range of topics Health Matters has covered (other recent editions have looked at alcohol and tobacco use, cervical screening, child dental health and obesity/food environment) or sign up to receive the latest updates through our e-bulletin.
And if you found this blog helpful, please view other Health Matters blogs.
Health Matters
Health Matters is a resource for professionals which brings together the latest data and evidence, makes the case for effective public health interventions and highlights tools and resources that can facilitate local or national action. Visit the Health Matters area of GOV.UK or sign up to receive the latest updates through our e-bulletin. If you found this blog helpful, please view other Health Matters blogs.

2 comments
Comment by Dennis Gore posted on
We know that:
“Coughs and sneezes spread diseases,trap your germs in a hankychief”.....a famous punch line from decades ago....
We also know that when you wash your hands it should take as long as it takes to sing the chorus :
“Happy birthday to you,happy birthday to you,happy birthday dear (your name) happy birthday to you!” TWICE!
We know that you should wash your hands after going to the toilet .
We also know you should wash before handling ,preparing food.
We also know to wash your hands when coming in from the garden.
Wash your hands after cleaning and dusting and using a vacuum cleaner etc....
BUT ,we are told,if you are TOO clean your immune system never has a chance to do it’s job of enabling you to build up a strong immune system,anti bodies etc.....
.....and yet household bleaches KILL 99% of germs!so,If your Immune System, in that scenario, will never have the chance to meet the germs and get it’s training which WOULD enable it to kill germs when needed!
So the question is:
What do microbiologists, surgeons, intensive care specialists,dentists,nurses,professors with qualifications in public health who give advice,what do they all “do” in their day to day lives with regard to the above questions?
Comment by Paul O'Hara posted on
Personally I think that the 50% goal by 2021 to reduce antibiotics being prescribed inappropriately does not go far enough. However, I do believe the World Health Organisation's Global Action Plan needs drive to run concurrent with the initiative. In particular Objective three: which calls for a reduction on the incidences of infection through effective sanitation, hygiene and infection prevention measures.
Dame Sally Davies recently stated that HCAI reported infections could be as high as 700,000 cases in the UK, over the previously unacceptable level of 300,000 annual cases. If the lower number is thought to cost NHS over £2Billion annually then aggressive action needs to happen and happen quickly!