
A little over a year ago, I wrote to the chief executive of every NHS Trust in England, calling for their personal commitment to work with PHE towards a truly smokefree NHS.
Now, I am writing for a second time, thanking all involved for the positive action that’s been taken towards making the ambition for a smokefree NHS an everyday reality.
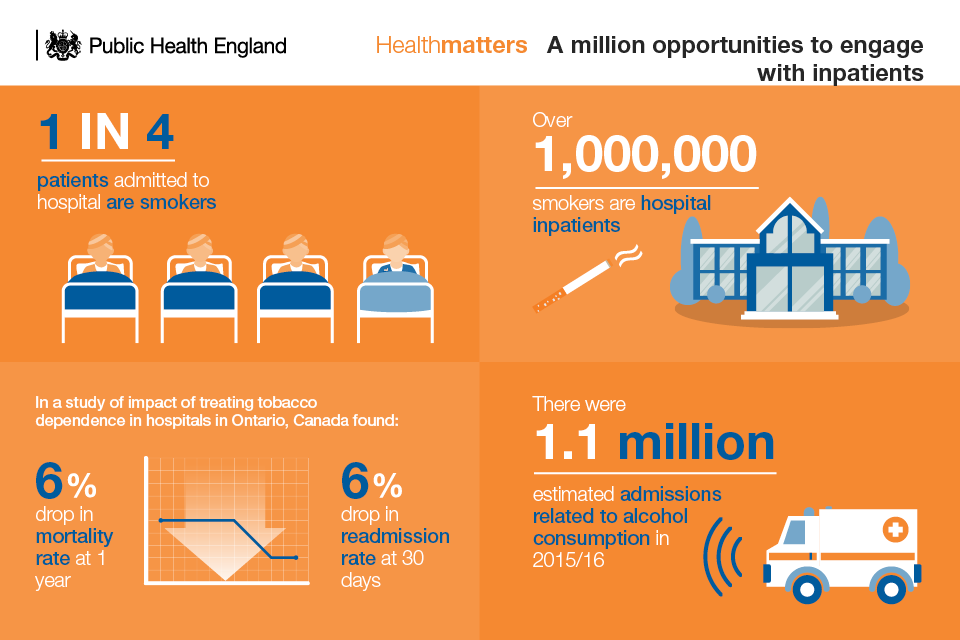
The NHS must be front and centre for us to secure a smokefree generation in England. One in four patients in hospital beds are smokers. Not only should the NHS be leading by example, but taking every opportunity to engage those patients that smoke.
One way to help tackle inequalities
Creating a smokefree NHS is one key way of engaging with typically hard-to-reach groups. Many longer term smokers will already be in poor health and in regular contact with their GPs, local hospital and wider community health services; this will also be true for many people with mental health problems, as well as pregnant women.
I have highlighted previously how smoking remains the leading cause of premature death in the UK and is responsible for half of the health gap between the poorest and most affluent communities. And, the latest analysis conducted by PHE and the Office for National Statistics shows the true extent of this inequality.
Looking at several measures of inequity, the analysis identified area deprivation as the factor with the biggest impact on someone’s likelihood of smoking.
Individuals living in the most deprived areas of England were more than four times more likely to smoke than those living in the least deprived areas.
Several other groups are also more likely to smoke, including:
- men, who are around 25% more likely to smoke than women
- people living in rented housing, who are more than 3 times as likely to smoke as those living in other housing types
- people working in routing and manual jobs, who are more than 3 times as likely to smoke as those in managerial and professional roles
- people with limited physical activity or who would consider themselves to be in bad health, who are around twice as likely to smoke as those with no limited activity or in good health
- people with no qualifications, who are around twice as likely to smoke as those with qualifications
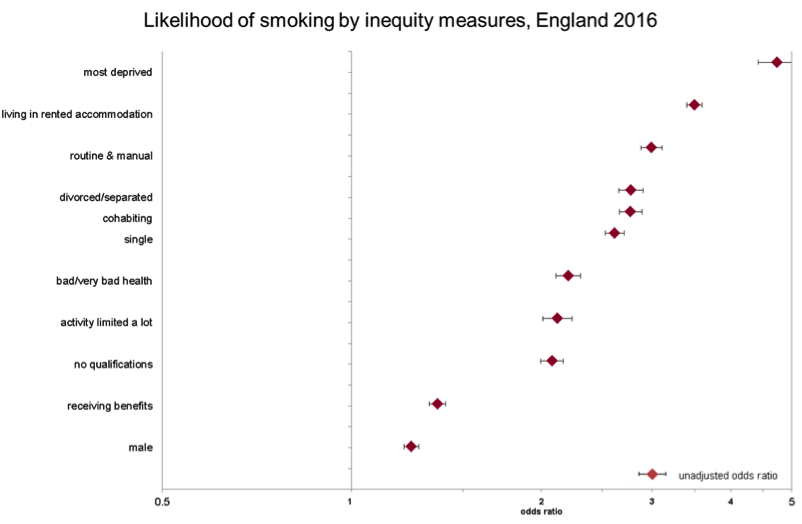
Characteristics such as sex, age, ethnicity, sexual identity, housing type and general health accounted for around half of the difference in smoking prevalence between the most deprived and least deprived areas.
But, even taking these into consideration, the most deprived group still have twice the odds of being a smoker compared to the least deprived groups.
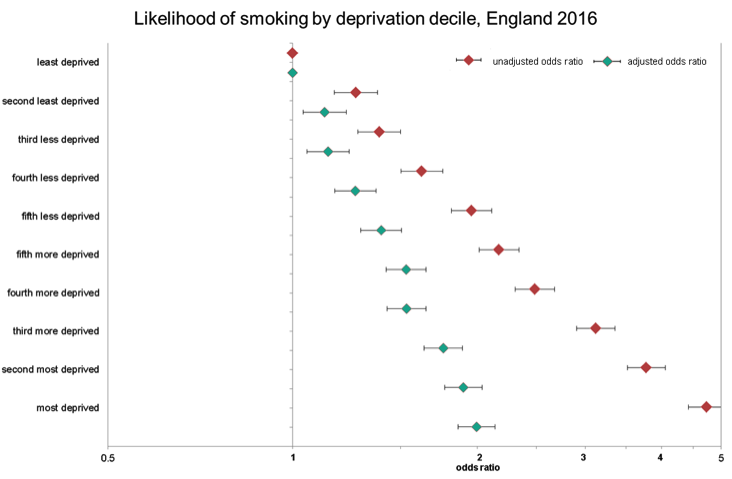
Adjusted odds ratios accounting for age, sex, ethnicity, religion, occupation, marital status, sexual identity, general health, disability, qualifications, housing type and benefits status.
Although we have seen progress between 2012 and 2016, the commitments to creating a smokefree NHS in the Tobacco Control Plan and the NHS Five Year Forward View are an important piece in the jigsaw of tackling health inequalities.
- In England’s most deprived areas, 27.2% of adults were smokers in 2016, down from close to one-third (32.7%) in 2012
- In England’s least deprived areas, just 7.9% of adults were smokers in 2016, which had decreased from 10% in 2012
That is why, in my letter, I especially commend the 90 per cent of mental health services who have already adopted the Preventing Ill Health by Risky Behaviours – Alcohol and Tobacco CQUIN, and many acute services are also implementing this—training staff to develop brief advice skills as an integral part of patient care, and agreeing local pathways for patients to receive smoking cessation support.
Implemented well the CQUIN has the potential to reduce future hospital admissions and reduce the risk of a number of chronic conditions such as heart disease, stroke and cancer. The Ottawa model has shown just how effective stop smoking advice can be when offered to every person admitted to hospital regardless of why they are admitted – those who received smoking cessation advice in hospital were more likely to have given up smoking after 6 months and less likely to be readmitted to hospital for any cause after 30 days.
Next steps towards tackling these inequalities
Of course, implementing such a change is not without its challenges. 1 in 4 patients admitted to hospital smoke, most of whom want help to quit and require strong and visible leadership at all levels within the NHS.
What’s clear from the data is that targeted efforts are needed to ensure we can reach our ambition of a smokefree generation.
The actions set out in the Tobacco Control Plan focus at the local level, prioritising more deprived areas and manual workers, vulnerable and young pregnant women, people with a mental health problem, and prisoners.
PHE and NHS England are working together to support acute and mental health trusts and all frontline health staff to become smokefree, and take every opportunity to encourage anyone using, visiting and working in the NHS to quit.
As part of this work, we are keen to find out more about each hospital’s smokefree policy, the support they offer and how it’s working in practice. We are therefore piloting a survey of Trusts across the South of England to better understand their current smokefree status, with a view to extending the survey across England later in the year.
We look forward to understanding more about how Trusts are progressing and sharing their achievements as we move towards a smokefree generation in England.
Our previous blog gives more detail on PHE’s role in delivering the Tobacco Control Plan.
Further analysis from this project can be seen on the ONS Visual website.

3 comments
Comment by Jo Flooks posted on
Not sure Mid Yorks Trust is aware of this. They have no smoking signs up around main entrance yet patients and visitors blatantly smoke whilst standing in front of these signs meaning staff and visitors have to walk through clouds of smoke to get in and out of the hospital. There's a smoking shelter a stones throw away but that's too far for them to walk when pushing a drip stand! I detest having to walk through second hand smoke without choice. Security staff turn a blind eye and let them get on with it.
Comment by Jane Hager posted on
Why is the pilot taking place in the south of England when figures for smoking are worse in the north? Also, smoking cessation services have been cut and inadequate information is being filtered to staff on the frontline as to why this is. This sends a message out that smoking cessation isn't a priority. If the plan is for front line staff to offer smoking cessation advice then training should be a consideration.
Comment by Mark O'Brien posted on
As a Service Manager for a Stop Smoking Service I see the above comment and behaviour highlighted by Jo Flooks at every hospital I visit. Unless this problem is managed from the top down then this will not improve as I have witnessed staff talking to patients whilst they are smoking in front of the very large No Smoking sign! The Smoke Free NHS is a fantastic idea as explained in the article above, and your local Stop Smoking Service should be able to assist you with achieving this goal.