Welcome to the latest edition of Health Matters, PHE’s professional resource. This edition focuses on some of the actions that local areas can take to reduce health inequalities experienced by people living with mental illness, so that they achieve the same health outcomes and life expectancy as the rest of the population.
Mental health problems can affect anyone and have a significant effect on the lives of individuals, their families, communities, and wider society. Together with substance misuse, mental illness accounts for 21.3% of the total morbidity burden in England.
One in 6 adults have had a common mental health disorder, such as anxiety, in the last week, at any one time according to survey data. Three quarters of mental health problems are established by the age of 24.

Severe mental illness (SMI), such as psychosis and bipolar disorder, affects close to an estimated 551,000 people in England. These individuals have a life expectancy of up to 20 years shorter than the general population and evidence suggests that the mortality gap is continuing to widen.
Poor mental health also impacts wider society, with it estimated to carry an economic and social cost of £105 billion a year in England.
Mental illness and inequalities
Mental illness is closely associated with many forms of inequalities, which people living with SMI are particularly vulnerable to experiencing. These inequalities are largely driven by complex and interrelated factors, including:
- wider social and environmental determinants of poor health, including poverty, unemployment, homelessness and incarceration
- stigma, discrimination, social isolation and exclusion
- increased behaviours that pose a risk to health such as smoking and poor diet
- lack of support to access health and preventative care
- diagnostic overshadowing – the misattribution of physical health symptoms to part of an existing mental health diagnosis, rather than a genuine physical health problem requiring treatment
Physical health inequalities amongst people with mental illness
People with mental illness also experience a greater burden of physical health conditions, often driven by the inequalities that they face. It is estimated that for people with SMI, two in three deaths are due to physical illnesses such as cardiovascular disease, and can be prevented. People with SMI are also more likely to have multi-morbidities, with younger adults with SMI being five times more likely to have three or more physical health conditions compared to all patients of the same age.
Furthermore, excess premature mortality rates are more than three times higher amongst people with mental illness in England compared to the general population, with recent analyses suggesting that this gap is widening.
The common behavioural health risk factors
Smoking remains the largest single cause of preventable death in England. Whilst smoking prevalence in the general population is at an all-time low at 14.9%, amongst people with SMI registered with a GP, it is almost three times that at 40.5%.
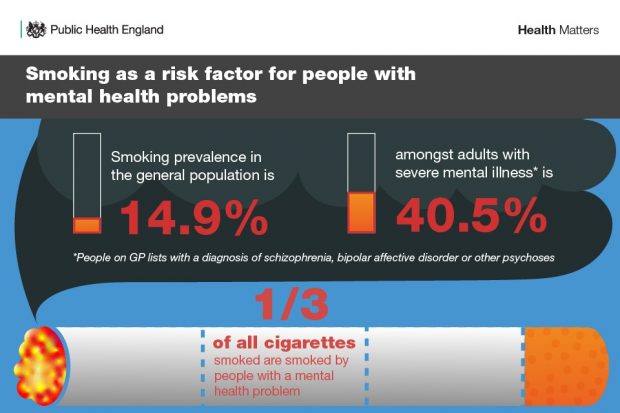
The Tobacco Control Plan for England recognises the need for urgent action in inpatient and community mental health settings to reduce this stark difference in smoking rates, and ensure people with a mental health condition are not left behind as we move towards a smokefree generation.
Preventative care and support for people with mental illness
Although people with SMI experience more risks to remaining in good health, they are not always offered timely and appropriate health assessments for early detection of physical health conditions.
Creating the right conditions for good health and wellbeing will require taking a whole person approach, addressing the root causes of poor health amongst people with mental illness, and empowering people to make informed choices. This will need system wide action at both a local and national level, with targeted action for those most at risk.
Read this latest edition of Health Matters to find out about the preventative actions that local areas can take to reduce inequalities and improve health outcomes and the lives of people with mental illness. This includes:
- understanding local population need
- addressing the social determinants of poor health
- early detection and intervention for physical health risks
- building a confident, competent and committed public mental health workforce
Visit the Health Matters area of GOV.UK or sign up to receive the latest updates through our e-bulletin. If you found this blog helpful, you can read other Health Matters blogs.


8 comments
Comment by Les Rogers posted on
Good common sense article, Just needs the will and resource to turn into a working reality.
Comment by Liz Robinson posted on
Would of been great to see a recognition of the impact of the coexistence of mental health and substance misuse disorders and the inequalities which exist in accessing services for this group. Plus signposting to good practice to resolve these issues.
Comment by Blog editor posted on
Thanks for your comment Liz. you can find a bit more information on the coexistence of mental health and substance misuse disorders in the full Health Matters content: https://www.gov.uk/government/publications/health-matters-reducing-health-inequalities-in-mental-illness/health-matters-reducing-health-inequalities-in-mental-illness
Comment by Karen English posted on
I work for a very small charity which supports people with enduring mental illness in their recovery. We use therapeutic gardening and rural crafts to build confidence and self esteem, together with employment coaching and benefits support. Despite PHE recommendations, budgets for mental health provision are being cut. This is significantly impacting people's lives and we find ourselves plugging gaps where core services should be. Less than a third of our funding comes from Mental Health Partnerships. Despite this, we know we make a difference. Imagine if there could be more of it.
Comment by Judith McGarty posted on
Diagnostic overshadowing; didn't know there was a name for this which is experienced by a close relative with long-term psychosis. As he ages he always attributes ill-health to his m/h symptoms or to his medication. Very hard to persuade him to go to GP. I have no formal role / patient confidentiality.
Also medicines: several times pharmacy have failed to deliver timely because 'waiting to complete the order'. Missing a day or two can be costly to his wellbeing. They don't seem to grasp importance. He is meticulous in ordering ahead despite all his problems thankfully.
Comment by Bhadri posted on
Impressive article.
Early intervention for prevention of physical and mental health condition.
Need of the community involvement.
However the community involvement in health promotion activities is a matter of behavior change. It sometimes become a challenge considering social ,economical and cultural boundaries.
Hard to reach population is another challenge.
Level of stigma in own community is a barrier .
In my opinion the stakeholder Luke community leaders , trusted person , health professionals.of the same community are well listened in my community.
Comment by Diane Clay posted on
Healthy habits need to be learnt in the early years and homes where these are taught and life is free from addictive behaviour and abuse will enable people to grow up with good mental and physical health. Where this is not possible I feel that children should be identified as needing extra care. This could be provided by people becoming evening foster carers, where children can go after school to enable them to experience the proper parenting, educational help and nutrition that deprived children need. I am trying to start a scheme called 'Extras' to do this. It is an attempt to break the 'cycle of deprivation' and provide needy children with the same advantages that other children have. My name is Diane Clay, I am a retired headteacher and would like people to e-mail me if they are able to help in any way. I live in Bedford. I was the deprived child of alcoholic parents, know a lot about how children can be helped.
Comment by john posted on
Thanks for this informative article. It was really very helpful for me. I got to know that smoking causes mental illness and also it is dangerous for health.