
The latest edition of Health Matters, PHE’s professional resource, focuses on the prevention of 5 common sexually transmitted infections (STIs): gonorrhoea, chlamydia, syphilis, genital herpes and genital warts. It also covers the public health challenge of antimicrobial resistant STIs, and the commissioning and improvement of sexual health services.
This blog provides a summary of the full edition’s content.
What is the scale of the problem?
STIs are a major public health concern, which may seriously impact the health and wellbeing of affected individuals, as well as being costly to healthcare services. If left undiagnosed and untreated, common STIs can cause a range of complications and long-term health problems, from adverse pregnancy outcomes to neonatal and infant infections, and cardiovascular and neurological damage.
In 2018, there were 447,694 new diagnoses of STIs made at sexual health services (SHSs) in England, a 5% increase since 2017 when 422,147 new STI diagnoses were made. Of these, the most commonly diagnosed STIs were:
- chlamydia (49% of all new diagnoses)
- first episode genital warts (13%)
- gonorrhoea (13%)
- first episode genital herpes (8%)
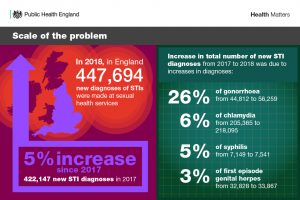
Gonorrhoea and syphilis have re-emerged as major public health concerns, especially among gay, bisexual and other men who have sex with men (MSM). In 2018, 47% of gonorrhoea and 75% of syphilis diagnoses were in MSM. Since 2009, gonorrhoea and syphilis diagnoses have risen by 249% and 165%, respectively overall, and by 643% and 236% among MSM. Higher risk behavioural changes, including more condomless sex with new or casual partners, likely contribute to these trends.
The diagnosis rates of STIs remains greatest in young heterosexuals aged 15 to 24 years, black minority ethnic (BME) populations, MSM, and people residing in the most deprived areas in England.
Preventing common STIs
This edition of Health Matters focuses specifically on the prevention of common STIs, as prevention is central to achieving good sexual health outcomes.
Prime responsibility for prevention rests with local authorities, who commission and support a range of work, often working collaboratively with PHE and the NHS.
The prevention work covered in this edition include:
- open access to SHSs, in person or online
- relationships and sex education (RSE)
- PHE’s national HIV Prevention and Sexual Health Promotion programme
- the National Chlamydia Screening Programme (NCSP)
- the National HPV Immunisation Programme
- the Syphilis Action Plan
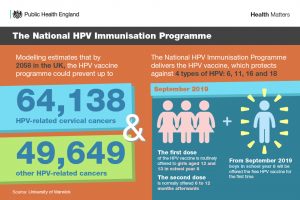
For example, the National HPV Immunisation Programme is a preventative measure as it delivers the HPV vaccine, which protects against 4 types of HPV. These include both high- and low-risk types responsible for the majority of cervical cancers and genital warts. By 2058, the programme could prevent up to 64,138 HPV-related cervical cancers and almost 50,000 other HPV-related cancers.
Antimicrobial resistance in STIs
Increasing resistance and decreasing susceptibility to antimicrobials used to treat STIs has reduced treatment options, and are therefore emerging concerns.
This is particularly the case for gonorrhoea, as there are no classes of antimicrobials to which gonorrhoea has not developed resistance. As a result of this, first-line gonorrhoea treatment in the UK was recently changed from dual therapy of ceftriaxone with azithromycin, to monotherapy with ceftriaxone at a higher dose.
Fortunately, ceftriaxone resistance remains rare in the UK. However, in 2018, there were 3 cases of extensively drug-resistant gonorrhoea detected in the UK, which included ceftriaxone resistance.

With patterns of antimicrobial resistance (AMR) having the potential to change rapidly, ongoing monitoring of AMR is vital to ensure that first-line treatment remains effective. Ineffective treatment facilitates onward transmission and adverse sequelae.
Collaboratively commissioning SHSs
Responsibility for commissioning sexual health, reproductive health and HIV services is shared across local authorities, clinical commissioning groups (CCGs) and NHS England. These shared responsibilities require a whole system approach to commissioning of these services. PHE and others have published a range of guidance to support this approach, which you can find in the full edition online.
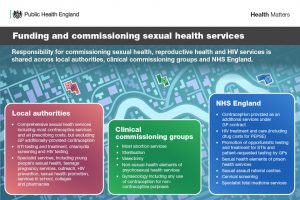
The recently published Prevention Green Paper outlines that government would like to see the NHS and local authorities working more closely at both the national and local level to make collaborative commission the norm, building on best practice from across the country.
It also sets out that the shift towards Integrated Care Systems (ICSs) creates the opportunity to co-commission an integrated sexual and reproductive health service. There are different ways of taking collaborative commissioning forward and each local area should decide what suits them best, using their existing powers and levers to develop joint approaches.
Call to action
The full edition suggests several calls to action for preventing STIs, including:
- preparing for the implementation of relationships education and RSE at primary and secondary level, respectively
- using condom distribution schemes
- using data, evidence and PHE’s resources including health economics tools to support decisions around commissioning SHSs
- commissioning collaboratively and whole-system working between commissioners
- delivering testing and treatment using existing frameworks and pathways, such as the chlamydia care pathway
- managing local STI outbreak and incidents with the support of PHE’s national guidance and national reference laboratory
Visit the Health Matters area of GOV.UK or sign up to receive the latest updates through our e-bulletin. If you found this blog helpful, you can read other Health Matters blogs.
