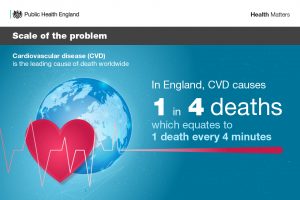
Cardiovascular disease (CVD) continues to be the leading cause of death worldwide and in England alone, it causes 1 in 4 deaths.
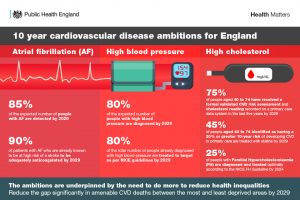
We are now one year on from when the National CVD Prevention System Leadership Forum (CVDSLF) – made up of 40 organisations and convened by PHE – agreed a set of national ambitions for the detection and management of the high-risk conditions over the next 10 years, known as ‘the cardiovascular ABC’s:
- Atrial fibrillation
- Blood pressure
- Cholesterol
This blog outlines several promising areas of work and initiatives led by members of the CVDSLF that have been addressing the ABC ambitions since their launch in February 2019.
Working with system partners
A whole systems approach to CVD prevention has continued to develop this year, whereby it is not only the ‘traditional’ clinical professions in this field that are working to detect and manage the ABCs in the general population.
For example, a range of community partners in Cheshire and Merseyside (C&M) are using a common approach to carrying out blood pressure checks. Cheshire Fire and Rescue Service (FRS) undertook an initial pilot to include blood pressure checks within their Safe and Well Checks and in February 2019, the approach started to be rolled out amongst the whole C&M FRS.
You can find out more about this work in this case study on blood pressure testing outside of general practice.
NHS England and Improvement's atrial fibrillation (AF) demonstrator programme is also taking the approach of working with different systems partners. In 23 Clinical Commissioning Groups (CCGs) across the country, specialist anticoagulation pharmacists or nurses have been working with GPs using a virtual clinic to identify and treat up to 20,000 people with high-risk AF who are not currently taking anticoagulants. It is estimated that this work could prevent up to 700 strokes and approximately 200 deaths from stroke between January 2018 and when the programme ends in March 2020.
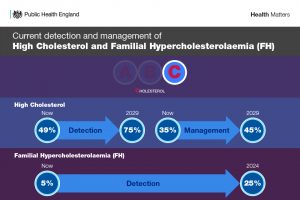
The British Heart Foundation (BHF) has also been supporting this approach with the introduction of a programme of systematic cascade testing for Familial Hypercholesterolemia (FH). Through this testing, in 2019, BHF funded nurses identified 1,094 people in England with FH.
You can read more about the work of two CCGs involved in this programme in this case study.
Promoting a holistic approach to prevention
The CVDSLF promote a holistic approach to prevention as instrumental in achieving these ambitions. This means that it is recognised that many people may be living with multiple overlapping conditions or risk factors, rather than just one of the ABC conditions or risk factors in isolation.
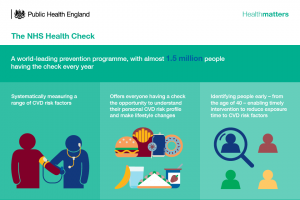
The NHS Health Check has been promoting systematic identification of risk and undiagnosed disease since the programme started in 2009, as all adults in England aged 40-74 who do not have pre-existing heart disease – or a range of other chronic conditions – are eligible for a check. Designed to spot early signs of stroke, kidney disease, heart disease, type 2 diabetes or dementia, the programme takes a holistic approach to preventing ill-health and premature death as we age. More than 8.1 million checks were completed over 6 years (April 2013 to March 2019).
In summer 2019, the government announced a review of the programme to enhance the offer and extend the reach of the existing service.
Enabling community mobilisation
Much of the CVDSLF’s work since the ambitions launched has focused on mobilising the community to understand and take care of their cardiovascular health.
With the aim of improving the public’s understanding of the risks of hypertension and easing the pressure on GP surgeries to accurately diagnose and manage the condition, the BHF spent £1.5 million on funding 15 programmes that involve wider community approaches to blood pressure testing. These programmes reach out to the local population through a variety of routes, from working with football clubs to setting up checks in supermarkets, and are changing the way people think and talk about hypertension.
Successful communication campaigns such as May Measurement Month and Blood Pressure UK’s Know Your Numbers week encourage adults to know their blood pressure numbers and take the necessary action to reach and maintain a healthy blood pressure, and has helped identify people with undiagnosed hypertension.
Advancing technology and innovation to enable the care agenda
In the past year, we also saw advancements in the application of technology that enables the detection of the ABC conditions or risk factors, which are being used in an increasing number of settings.
Driving the advancement and democratisation of technology in this way links in with the community mobilisation and working through systems partners approaches, as it allows a range of professions and the public to detect and manage their own risk factors.
Academic Health Science Networks (AHSNs) have contributed to this prevention agenda, for example through leading a national roll-out of hand held electrocardiogram devices to help identify people with AF and introducing technology to help people with AF self-test their international normalised ratio (INR) levels. AHSNs will continue to contribute to this agenda in support of the CVD prevention ambitions, with future innovations involving things such as point of care tests for cholesterol and Apps which can accurately measure blood pressure.
Using data and evidence to drive improvements
This year, there has been an emphasis on the role of data and evidence for driving improvements in addressing the ABCs.
In 2019/20, NHS RightCare received national clinical support to deliver National Priority Initiatives on CVD prevention. NHS RightCare is working with NHS England’s National Clinical Director for CVD Prevention, the BHF, PHE and the National Institute for Health and Care Excellence to ensure a clinically-led approach, which focusses on:
- optimal management of known patients with AF
- optimal management of known patients with hypertension
Having national clinical priority status has helped to ensure that 82% of CCGs have an action plan to address AF and 78% have an action plan to address hypertension.
NHS RightCare’s Atrial Fibrillation High Impact Intervention Tool was developed in collaboration with Imperial College Health Partners to support local health systems to measure the value of identifying and treating patients with AF. This includes estimating the budget impact of screening and treatment-based interventions, which subsequently helps with creating an exportable business plan for treating AF to be used locally.
In October 2019, PHE and NHS Digital jointly published for the first time an interactive data dashboard on NHS Health Check primary care data. This dashboard provides the number of patients attending an NHS Health Check between April 2012 and March 2018, using data recorded by participating GP practices. Data on over 10 million patients can be broken down by age, sex, ethnicity as well as local authority and CCG. The richness of this data is significant and will help to improve understanding of the NHS Health Check programme’s impact and inform what action is needed to improve service delivery and outcomes.
This year has also seen improvements in access to and visibility of data with the commitment to establish CVDPREVENT – a national primary care audit that will automatically extract routinely held GP data covering diagnosis and management of six high-risk conditions that cause stroke, heart attack and dementia. CVDPREVENT will provide a foundation for professionally led quality improvement in individual GP practices across Primary Care Networks (PCNs). It will support primary care in understanding how many patients with the high-risk conditions are potentially undiagnosed, under treated or over treated, in turn allowing identification and monitoring of inequalities.
The NCVIN have developed Sustainability and Transformation Partnership (STP) level CVD Prevention Packs to estimate the local contribution to the CVD prevention national ambitions. These include information on the variation in hypertension and atrial fibrillation diagnosis and management at STP, CCG and GP level. The packs are currently undergoing their third update and will include updated hypertension prevalence information.
Publishing guidance and educative material
This year, the All Our Health CVD prevention module and an interactive e-learning version of the topic were published, which aim to increase the confidence and skills of health and care professionals to embed prevention into their day-to-day practice. It provides action points for front-line health professionals to:
- identify and manage CVD risk factors
- understand local needs using data through PHE’s National Cardiovascular Intelligence Network
- measure impact and demonstrate the value of their contribution
PHE also published a blog – What you need to know about statins – which focuses on the types and dosages of statins and the current prescribing guidelines. Importantly, it clarifies the common controversy that statins attract, for both health and care professionals and the public.
NICE refreshed their guidance for the diagnosis and management of hypertension in adults this year, which is for healthcare professionals, commissioners, providers, and people who have or may have high blood pressure, as well as their families and carers.
PHE and the Association of Directors of Public Health have collaborated to publish a series of What Good Looks Like publications, which set out the guiding principles of what good quality looks like for population health programmes in local systems. They aim to be a practical resource for leaders and practitioners in the public health system in England and include a publication on CVD prevention.
What’s next?
These are just a few examples of work that the organisations represented by the CVDSLF have led on this past year. As such, it is clear that in the first year since the CVD prevention ambitions were launched, promising progress has already been made towards achieving them.
In order to retain this momentum, it is important that we continue to promote a whole systems approach, as there are many other parts of the system in addition to primary care that can find the people most at risk of developing CVD. Furthermore, we must regularly monitor our progress and CVD diagnosis and management in England and with this in mind, we look forward to what the CVDPREVENT audit – commissioned by NHS England and NHS Improvement – reveals to us.
Fundamental to achieving the ambitions is also the need to drive reductions in the gap in avoidable CVD mortality and morbidity between the most and least deprived, as well as in wider population groups that are living with more risk factors and impacted the most by CVD. This target should therefore continue to underpin all ongoing and future initiatives that tackle the ABC risk factors.
For more information, you can sign up to our CVD prevention team’s e-bulletin.
For more on the CVD prevention ambitions and the scale of CVD in England, read PHE’s edition of Health Matters from February 2019, which launched the ambitions.
