
A new decade brings fresh opportunities to look at how, as a nation, we can tackle inequalities in health.
Ten years on from his original report, Michael Marmot and the Institute of Health Equity have produced a new and important contribution to this debate.
The report highlights areas of continuing concern and calls for further action at many levels.
There is existing cross system activity on health inequalities but it is clear that more needs to be done.
We look forward to new commitments to addressing geographical variation in health outcomes in the Government’s forthcoming response to the green paper ‘Advancing our health: Prevention in the 2020s’.
And alongside this, the NHS Long Term Plan has already made a welcome and firm commitment to a more concerted and systematic approach to reducing health inequalities and addressing unwarranted variation in care.”
In this blog we look at some of the work PHE is doing to reduce health inequalities, including the developing priorities set out in our new 5-year strategy for 2020-2025.
Reducing health inequalities
Reducing health inequalities means giving everyone the opportunity to lead a healthy life, no matter where they live or who they are.
It’s well documented for instance that in England, people living in the least deprived areas of the country live around 20 years longer in good health than people in the most deprived areas.
As well as being unfair, health inequalities are costly, putting a strain on employment and productivity, affecting national and local economies and impacting on our public services.
So how do we tackle these unfair and avoidable differences in health across the population?
Communities and places matter
The environments in which we’re born, live and work really matter for health. A good education, a decent job, a suitable roof over our head, friendships and networks to feel part of – these are the ingredients for a healthy life.
It’s because these social and environmental factors are so important that local government and local areas have such a crucial role to play, forging alliances across their community that boost wellbeing and reduce inequalities.
We want to support the efforts of local areas, and with this in mind we recently published Place-Based Approaches for Reducing Health Inequalities working with our partners at the LGA and ADPH.
The set of resources provides a practical framework and tools helping places to reduce health inequalities using civic, service and community interventions.
We are now piloting support to Integrated Care Systems and Health and Wellbeing Boards across the country to adopt the tools and principles of this work.
We developed the resource further in January, publishing new research on community-centred approaches to improve health and wellbeing, an important aspect of a place-based approach to reducing inequality.
Other recent guidance focussed on place, includes our evidence summary of health inequalities among older people in coastal and rural areas and a guide to using the planning system to promote healthy weight environments.
Throughout this year we’ll publish more guidance which helps local areas make the case for tackling the root causes of poor health, including a review on improving access to greenspace later this month.
Look out also for a future edition of Health Matters on housing and health, along with resources focussed on getting public health research into planning practice, and using health impact assessments in town planning, all due in the spring.
National work to narrow the health gap
PHE recently published a new 5-year strategy and in it we acknowledge that we must integrate the reduction of inequalities into everything we do in order to stand the best chance of tackling long-standing injustices and improve the health and wellbeing of the nation.
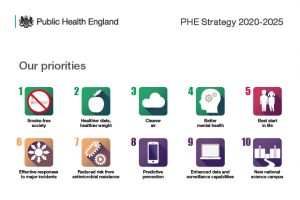
We selected our 10 priorities as they are areas where PHE is well placed to make a contribution with scope to improve outcomes and reduce inequalities.
For instance, our Smoke-free Society priority workstream will aim to reduce variation in smoking prevalence rates between socio-economic groups, particularly looking at routine and manual workers, pregnant women, people with mental health problems and people in contact with the health services.
And our Healthier diets, Healthier weight priority, which includes our food reformulation work and whole-systems approach to obesity initiative, seeks to reduce the gap in obesity rates between children from the most and least deprived areas
Our Cleaner Air priority can drive better health outcomes for vulnerable groups most affected by poor air quality and we will work towards ensuring mental health has parity with physical health, reducing inequalities in premature mortality for people with long-term and severe mental health problems through our Better Mental Health workstream.
The Marmot reports stress the importance of every child having the best start in life. To help reduce inequalities and improve health outcomes for children and families, PHE wants all mothers to experience good health before, during and after pregnancy and all children to have a happy healthy childhood. This is an ambition we’ll address through our Best Start in Life priority.
This blog can only provide a snapshot so please read our 5-year strategy for a flavour of how we’ll embed tackling health inequalities in the areas above, as well as our priorities on responding to incidents, AMR, predictive prevention, data and surveillance and the development of a new public health campus.
Our business plan for 2020/21, due later in the Spring, will look at our objectives as the strategy enters its first year.
Inclusion health and equalities
Tackling regional inequality is a vitally important task, but we also see differences in health linked to disability, gender, race, age, sexuality or religion or amongst members of the most vulnerable or marginalised groups in society from homeless people and sex workers to people in prison.
In our new infectious disease strategy, a companion document to our 5-year strategy, we identify pathogens which disproportionately affect groups already experiencing health inequalities.
Over the next 5 years we will build the evidence and focus on diseases that are prevalent in under-served populations including tuberculosis, blood borne viruses and other infectious diseases in homeless and prison populations.
Our work to reduce health inequalities for vulnerable groups recognises that these groups have very high needs and require targeted responses. We’re currently working on projects to improve the health of rough sleepers and substance misusers including testing models that can improve the health of people sleeping rough and have a well-established Health and Justice team.
We address this further in a recent Lancet piece ‘From health for all to leaving no-one behind: public health agencies, inclusion health, and health inequalities’.
Informing decisions with data
To support vital national and local action to reduce inequalities another key aspect of our work is offering a range of data.
Alongside the annual Health Profile for England which is designed to inform national policy we regularly update and improve tools like our Health Inequalities Dashboard, our Segment Tool and our Wider Determinants Tool. Our Health Inequalities Dashboard is being updated this March and will include some further analysis of geographical inequalities alongside it.
We are also refreshing our Health Equity Assessment Toolkit which helps professionals systematically assess equalities and health inequalities related to their work programmes.
Finding out more
To find out more or for further updates on this agenda please subscribe to this blog or follow us on Twitter. You may also find our Health Matters resource a useful source of information on health inequalities and the wider determinants of health. For instance, recent editions have looked at health and work and a lifecourse approach to prevention.
