
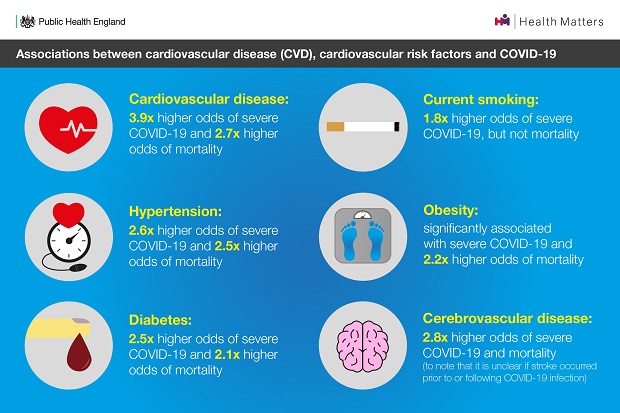
The evidence is clear, Cardiovascular disease (CVD) and COVID-19 share common underlying risk factors. People with pre-existing CVD, diabetes, obesity and high blood pressure are not only at greater risk of having a heart attack, stroke or developing some forms of dementia, but are known to experience more severe outcomes from COVID-19, including hospitalisation, ventilation and death.
What is more, they both disproportionately affect the most deprived communities. Out of the most common causes of death, CVD is the largest contributor to the gap in life expectancy between the most and least deprived, accounting for up to 25% of the difference. Data also shows that premature CVD mortality is four times higher in the most deprived communities.
Similarly, the severity of outcomes from COVID-19 are unequally distributed across society as it amplifies existing underlying health issues and deep-rooted health inequalities.
From March 2020 to January 2021, COVID-19 was one of the contributing causes of more than 2,750 CVD deaths. As the impact of COVID-19 continues to be assessed, it’s possible that we will also begin to see the impact of delayed access to the management of cardiovascular diseases. There will also be consequences for prevention. In particular from the significant reduction in provision of the NHS Health Check programme over the last 12 months which will greatly impact on the 240,000 people with obesity, 16,000 with high blood glucose and 250,000 with high blood pressure that the programme can identify and support each year.
However, it isn’t all bad news. COVID-19 has helped take the use of technology to a new level and opened opportunities for making better use of data. As we begin to plan recovery from this pandemic there is an opportunity to not only align action on CVD with COVID-19 recovery, but also ensure healthcare restoration is equitable and maximise the arising digital and data opportunities.
This is why the CVD national ambitions and the NHS Long Term Plan commitment to prevent 150,000 heart attack and strokes over the next 10 years, remain vital to recovery and restoration. Now two years on from when they were first published, these commitments remain just, if not more, relevant today.
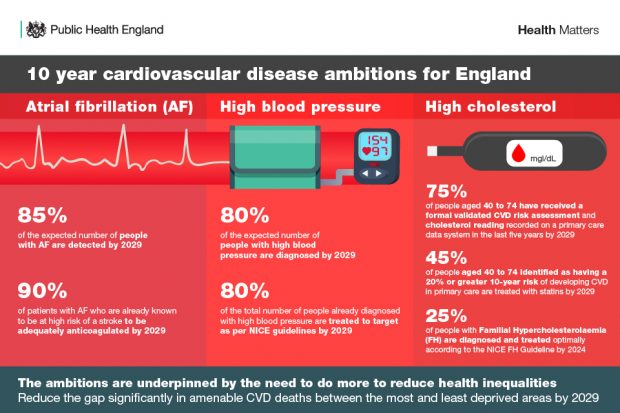
Over the last year, despite extremely challenging circumstances, many system partners have demonstrated amazing leadership in order to retain a focus on CVD prevention and deliver interventions against the three high impact areas of Atrial Fibrillation (AF), Blood Pressure and Cholesterol.
What has been achieved
In the last 12 months, NHS England and Improvement (NHSE/I)
- piloted the opportunistic detection of hypertension in community pharmacies. The pilot aims to target inequalities by reaching people who are not routinely in contact with NHS services and identifying those at high risk of CVD, who would otherwise go undiagnosed.
- In partnership with NHSX secured 22,000 blood pressure monitors prioritised based on deprivation to people in the COVID-19 clinically vulnerable category, enabling them, for the first time, to remotely monitor their blood pressure.
- Evaluated a virtual Atrial Fibrillation (AF) pilot which aimed to improve anticoagulation rates among people with an existing diagnosis of AF.
- Developed a Primary Care Network Directed Enhanced Service (DES) prevention specification on CVD which will be implemented from 2021/22.
The Academic Health Science Network (AHSN) and Accelerated Access Collaborative have focussed on accelerating the identification and management of people with Familial Hypercholesterolaemia (FH) by supporting the adoption of new models of care. UCL Partners have developed new prevention pathways for Hypertension, Atrial Fibrillation and Cholesterol. The Primary Care Cardiovascular Society and Oxford Academic Health Science network have developed a fantastic resource which provides information to primary care teams on how to overcome limitations presented by COVID-19 to deliver quality CVD prevention services.
This year has also seen a focus on improving access to and visibility of data. PHE and NHSE/I have continued work on CVDPREVENT, the national primary care audit that will support Primary Care Networks to target improvements by identifying where the management of high-risk conditions could be optimised. PHE’s CVD prevention packs have been refreshed to reflect data highlighting the local opportunities to support the delivery of the national ambitions at Sustainability and Transformation Partnership, Clinical Commissioning Group and General Practice level.
The British Heart Foundation (BHF) launched new hubs which have recorded over 3.5 million users and provide valuable patient information on COVID-19 and heart failure, weight loss, blood pressure and cholesterol. With over 12,000 views the AF Association and Arrhythmia Alliance educational video on the COVID-19 vaccine and anticoagulation therapy has also been well received. HEART UK has continued to support people with hyperlipidemia with helpline use increasing by 42% during the pandemic.
The National Institute for Health and Care Excellence (NICE) has published a collection of CVD prevention guidance specifically designed for local partnerships and a new impact report on CVD management, which contains a section on responding to COVID-19. The College of Podiatry supported its members by producing training modules on CVD, atrial fibrillation, blood pressure and cholesterol. HEART UK has delivered a series of webinars for healthcare professionals, including a lipid update which was attended by over 300 healthcare professionals.
The Stroke Association delivered the first ever Stroke Prevention Day engaging the public on reducing stroke risk and the Atrial Fibrillation Association’s social media campaign on AF detection and anti-coagulation encouraged the public to take action to reduce AF-related stroke. PHE joined other organisations in highlighting the need for further action on CVD prevention as part of a national cardiovascular health campaign.
There have also been great examples of local action. In Cheshire and Merseyside adaptations enabled action on CVD prevention to continue during the pandemic. This has included the development of local quality improvement tools for general practice, scaling up of remote blood pressure monitoring supported by digital solutions, webinars for primary care teams focussed on the three high impact areas, a sub-regional Happy Hearts website including translated and easy-read resources with over 10,000 new users and a social media campaign targeted to areas of deprivation which reached over 1.3million people.
Looking to the future
CVD, COVID-19 severity and health inequality are interconnected, and as such delivering the national CVD ambitions will benefit all three. As we emerge from the pandemic there is the challenge of dealing with its wider impact on health but also an opportunity to embrace new ways of working in order to build back better and fairer.
To achieve this, you can:
- Prioritise action on CVD prevention and the national ambitions in local COVID-19 recovery plans across local government, Integrated Care Systems, Clinical Commissioning Groups and Primary Care Networks.
- Adopt an approach which prioritises resources and equipment to the most disadvantaged areas.
- Target services at individuals in the most disadvantaged groups.
- Reimagine care pathways to take full advantage of technology in improving care pathways which seek to improve the detection, treatment and management of atrial fibrillation, high blood pressure and high cholesterol.
- Prioritise the recovery of CVD prevention programmes such as the NHS Health Check and explore new delivery models which will maximise the engagement of the most disadvantaged.
- Use data such as CVDPREVENT to understand the size of the health backlog and the gap between the detection and prevalence of AF, High Blood Pressure and High Cholesterol.
- Support practitioners to refresh CVD training and develop competencies in techniques such as motivational interviewing that will enable them to deliver a high-quality CVD intervention that empowers patients take action.
