At the Academy Awards earlier this year, Matthew McConaughey and Jared Leto won Best Actor and Best Supporting Actor for their respective portrayals of people living with HIV. I’m a scientist, not a film critic, but I couldn’t help but compare the Dallas Buyers Club with the lack of similarly insightful stories about people living with hepatitis C.
It’s a minor complaint, but it’s also symptomatic of the lack of understanding and awareness of hepatitis C infection. The World Health Organisation estimates 35.3 million people were living with HIV/AIDS worldwide in 2012, but up to 150 million people globally have chronic hepatitis C infection.
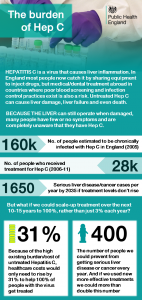
In England we have about 160,000 people chronically infected with hepatitis C. This virus causes inflammation of the liver, but because our livers can still operate when damaged, many people are completely unaware they have the infection.
The good news is that unlike many viruses, including HIV, we do have a way of clearing hepatitis C. We have hepatitis C treatment.
Treatment is not an easy road for everyone, but for the majority of people with hepatitis C, it represents a real opportunity to be clear of the virus and to live free from the fear of chronic liver disease and premature death. There are also new treatments on the horizon.
However, just 28,000 people received treatment between 2006 and 2011. That means only 3% of the people chronically infected with hepatitis C are accessing treatment each year. If we continue with these treatment levels of standard treatment, by the year 2035 England will be facing 1650 cases of hepatitis C-related end stage liver disease and cancer every year.
Our recent study published in the Journal of Hepatology looked at the cost of increasing hepatitis C treatment uptake in England, and the impact this would have on disease burden.
We modelled the total additional cost for scaling up standard treatment from 3% to 100% coverage over the next 10-15 years. You’d expect it to be a massive increase, however because of the burden of associated healthcare costs presented by untreated hepatitis C you’re only looking at a 31% increase over the amount we’re already spending.
It’s an increased overall cost yes, but one that comes with a bigger saving in terms of lives lost and disease burden prevented. Because high levels of treatment have the potential to reduce the prevalence of hepatitis C infection as well as the disease burden, increasing treatment is an important component of prevention activity too. If there is less hepatitis C out there, then it is harder to get infected in the first place.
As well as encouraging more treatment, there is also an urgent need for better monitoring and reporting of treatment outcomes, and expansion of treatment into non-traditional settings, such as primary care, drug treatment centres, and prisons. This would help us to tackle hepatitis C and address health inequalities by reducing the excess premature deaths from hepatitis C-related liver disease that are concentrated in marginalised populations.
And maybe that would be a hep C story worth telling.
Featured image copyright Public Health England. Used under Crown Copyright

8 comments
Comment by Annie Walker posted on
I have done the treatment 4 times and it returns each time. I do not think we have a treatment seeing as I am on the liver transplant list and still have the virus.
Comment by Helen Harris posted on
Really sorry to hear that; I know that current treatments are not effective for everyone. Do you know whether you are eligible to receive new direct acting antiviral drugs that have recently been made available on the NHS for a defined group of patients who are at significant risk of irreversible liver damage within the next 12 months? Not everyone is eligible, but it would be worth discussing with your doctor. http://www.england.nhs.uk/2014/04/16/hepatitis-c/
Comment by Anne walker posted on
I am starting sofosbuvir soon and consider myself very lucky to get the chance ( even though I was infected via NHS 35 years ago) but as a geno 3 with cirrhosis and being retreated the fabulously high 95% chance of clearance drop to 33% - or so I hear thus far.
Comment by Helen Harris posted on
Annie, I wish you the very best of luck with this treatment; let's hope this one will work for you.
Comment by Bill Carney posted on
I finished Hep-C treatment about 7 yrs ago. At first they said I don't need to be treated. A year or so later they said although not a lot of damage has occured, its better to go ahead and be treated. So I did, after 3 months it was undetectable, They continued for the entire 50 weeks and now I have been clear for 7 yrs, maybe a little longer. I get checked annually. So I guess I'm a success story. I'm also a Veteran. I was told 50% of all Vets who go to Fayetteville NC VA Hosp were Hep-C positve. Thats where I got treated,
Comment by Helen Harris posted on
It's good to hear that your treatment was successful, Bill; it is certainly true that treatment is successful for the majority of patients these days. New drugs are also on the horizon that offer the potential to improve response rates further.
Comment by Bren posted on
Hello Helen,
Thanks for the really good blog and the awareness you have delivered .
I think the trust and increasing uptake is hugely important and maybe we need to look at lessons learnt from other areas as to how best to do this in a sensitive, respectful, and supportive way.
Bets wishes and thank you,
Bren.
Comment by Helen Harris posted on
Absolutely, and we are working very hard with partners and stakeholders to try to improve things for patients. I hugely value the input that we receive from patient groups when we are working to improve services; it is important that patients remain at the very heart of things so we get services right.