We've published an evidence review of the outcomes that can be expected of drug misuse treatment in England, which was commissioned by the Department of Health in 2015 and has helped inform the forthcoming government Drugs Strategy.
How England drug treatment compares internationally
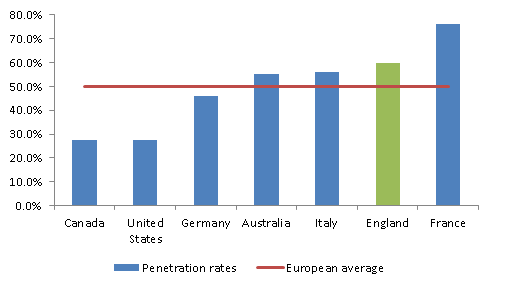
The evidence shows that where comparisons were possible, the treatment system in England is performing well - with 60% of all opioid users in treatment - among the highest treatment penetration rate reported.
Other areas where treatment outcomes in England are comparable with or better than other countries and compare well to the scientific literature included:
- access to treatment (97% within three weeks) is comparable to other countries
- the rate of injecting among all 15-64 year olds (0.25%) is relatively low
- the rate of drop out from treatment before three and six months (18% and 34%) is comparable to the literature (28% on average)
- a very low rate of HIV infection among injecting drug users (1%), which compares favourably internationally
- the rate of Hep C infection (50%) is lower than several other countries with available data
While largely positive, there are two key areas of concern that need improvement:
- the rate of opiate abstinence after three and six months of treatment (46% and 48%) points to relatively poorer performance in comparison with the literature (56% on average)
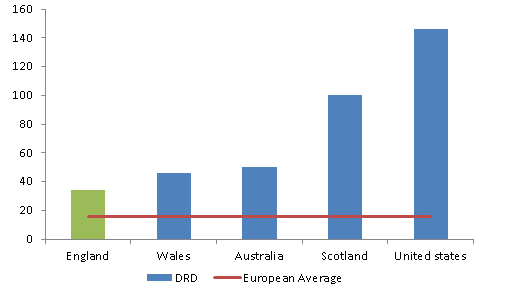
- the drug-related death rate (34 per million in 2013) is substantially lower than the USA but considerably higher than elsewhere in Europe. The rate in England has now increased to 42 per million in 2015 (Wales and Scotland have also seen an increase over this period)
The changing treatment population – future challenges
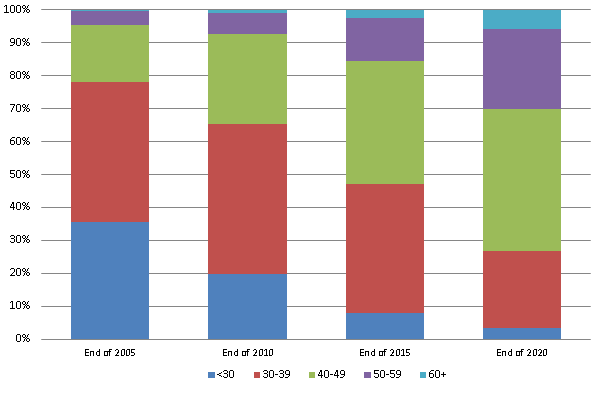
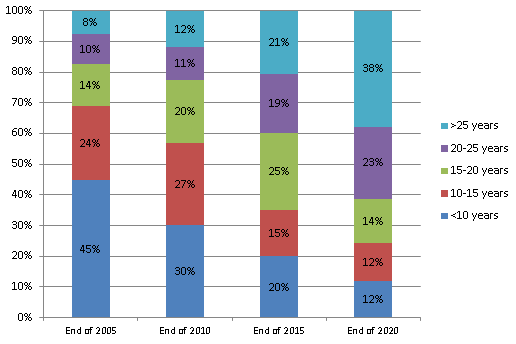
The majority (around 75%) of people currently in drug treatment in England have problems with opiates, mainly heroin. In recent years we have seen an increase in the proportion in treatment with entrenched dependence and complex needs, experiencing cumulative physical and mental health conditions and we expect this is likely to continue to rise.
This changing population of older heroin users will present challenges for services and local councils. They are less likely to successfully complete treatment and more likely to die from long-term conditions and overdose. It is important that we help this particularly vulnerable group to access appropriate general healthcare services and other forms of support.
Other challenges
There are reports of increasing problems of misuse and dependence associated with some prescription and over-the-counter medicines. The use of new psychoactive substances (NPS) is also a threat, and is a particular problem in prisons.
New patterns of drug use and health risk behaviour are also becoming established including injecting NPS use, and drugs used alongside high-risk sexual behaviour (‘chemsex’). These require close monitoring and responses that range from managing prescribing practices to developing the skills of professionals.
Social factors are important influences
The evidence also shows that social factors are important influences on treatment effectiveness. Areas of relatively high social deprivation have a higher prevalence of opiate and crack cocaine use and larger numbers of people in treatment. Unemployment and housing problems have a marked negative impact on treatment outcomes and exacerbate the risk that someone will relapse after treatment.
Specialist treatment services are vital but treatment cannot do it alone and further support is needed to help people into lasting recovery through employment, decent accommodation and strong social networks. It is essential that the local offer reflects the needs of the community and PHE provides a number of tools and expert data to support local authorities to deliver appropriate, tailored and effective services.
The benefits of investing in treatment
Drug misuse has a significant cost to society as a whole, costing the UK an estimated £10.7 billion each year from health service costs, drug-related crime and economic costs such as premature deaths. Investing in drug treatment can impact on these costs and it is estimated that every £1 spent on treatment yields a £2.50 saving on the social costs of drug misuse.
The evidence is clear that treatment affords individuals and communities many benefits. Continued investment in treatment and in ensuring services are fully integrated with other healthcare and social services will save local communities money and help to address health inequality.
While we celebrate the benefits of investment in drug treatment and recovery in the positive outcomes we see in England, the challenges going forward for local authority leadership, commissioners, treatment providers and for service users themselves remain:
- are we doing enough to reduce drug related deaths, particularly amongst users outside the treatment system and how are we managing ‘use on top’?
- are we satisfied that the majority dying are not engaged and are the harm reduction and crime reduction benefits of treatment sufficient that ‘use on top’ is acceptable?
Two priorities for the public healthcare system and PHE going forward.


1 comment
Comment by John Divney posted on
One thing that never gets mentioned is the effect that a good drug service, an inclusive drug service, one founded on sound Harm Reduction principles, can make to the town in which it is sited. Having our most troubled citizens treated effectively for their addiction then the hassle that that habit can create for the whole community is lessened. Families, school, crime, prison sentences, health and a whole range of other social issues are ameliorated. Once that service has been replaced by LA commissioners in the name of saving money, by a charity whose underpinning philosophy is Recovery then everything changes. CGL came to Birkenhead two years ago having replaced the NHS Wirral Drug Service for reasons unknown and unexplained. Birkenhead is now a dangerous and violent town and has gone back to what it was twenty years ago when scripts were once hard to find. Over the years the NHS service here excelled in the numbers of users they brought into, and more importantly retained in decent MMT. I have never seen so many homeless drug users, so many street drinkers who used to be in treatment with the old service, so many old bag-heads who again used to be in treatment with the old service, all hanging around doing what they do around the DHSS buildings and the cheap bakery shops and off licenses. We now have reports in local papers of used syringes being found in back alleys, alongside a constant flow of stabbings, gang fights and violent robberies. Its not been like this since the early 90s. I put the blame squarely at PHEs door for ensuring that recovery lies at the heart of National drug treatment and that charities like CGL and others are then commissioned by LAs with PHE advice, to get people out of treatment, most before their time and most before they are ready. This is helping no one least of all the people of Birkenhead/Anytown and the dead addicts whose numbers continue to grow to PHEs shame.