New Psychoactive Substances (NPS) have featured heavily in recent media stories, and are an increasing focus of our work in PHE.
Earlier this year the Home Office published a new Government Drug Strategy, and PHE is now leading on a number of key areas, particularly on NPS.
We recently shared our suite of resources and toolkit for management of NPS within prisons and the subsequent evaluation.
However, a gap remains in the evidence and literature around the impact of NPS in secure mental health units.
As part of our prevention programme for NHS England’s Specialised Commissioning Mental Health Programme of Care Board we have already undertaken work on smoking and obesity in these settings, and will now focus on NPS.
We reviewed the latest clinical evidence, and surveyed low, medium, high secure, and Child and Adolescent Mental Health Units in England on the current issues they were experiencing with NPS.
The results were striking and provide a strong case for continued public health action focused on patients with mental health conditions who are using, or have used NPS. Read the full report: A review of new psychoactive substances in secure mental health: summary document.
NPS use and clinical impact in mental health units
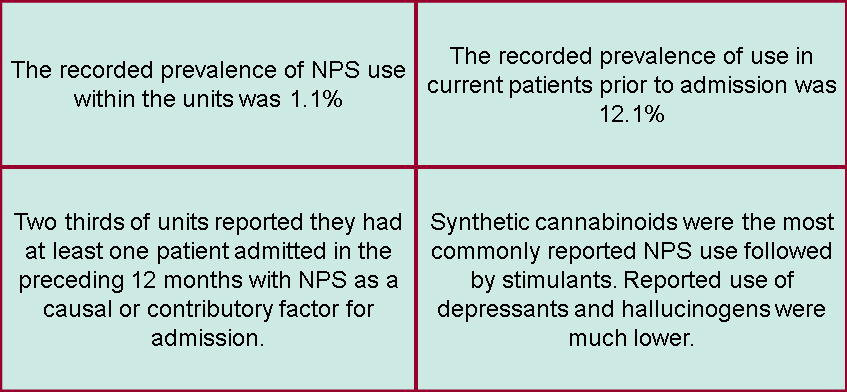
The survey found that current NPS use was relatively low (1.1%), however the reported prevalence of use by patients prior to admission was significantly higher (12.1%) (Fig 1). Two thirds of those recorded as using NPS were also recorded as using at least one other illicit substance.
The survey also asked questions about the physical and psychological symptoms of NPS, as well as their wider impact on the setting’s environment.
Physical symptoms most frequently associated with NPS were:
- cardiovascular symptoms
- reduced consciousness
- dizziness and vomiting
Psychological symptoms included:
- psychosis
- anger
- aggression and
- paranoia
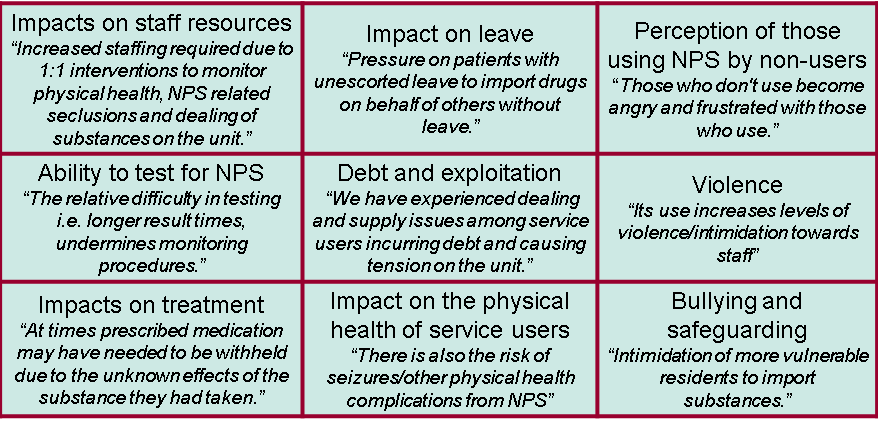
NPS also had a wider impact on mental health units including:
- impacts on staff resources
- trading and exploitation
- perception of those using NPS by non-users
- violence
- ability to test for NPS and impact on leave
Additional challenges noted by the units were; bullying and safeguarding, concerns about impacts on treatment and the physical health of service users. Figure 2 shows these themes with selected quotes from respondents.
What does the clinical evidence tell us?
In addition to the survey, we conducted an evidence review, which highlighted a number of themes related to the impact on NPS in secure mental health services.
The evidence, although limited due to the quality of studies available, highlighted that:
- NPS can induce psychiatric symptoms in those with no prior mental health diagnosis and can exacerbate symptoms in those with existing serious mental illness
- this may translate to an impact on admissions and care in secure mental health settings
- there is a clear correlation with longer length of stays in inpatient units with implications for bed utilisation and service delivery
- clinicians should be aware of the potential for NPS to induce mental health symptoms and how this can be diagnosed and treated
- patients should be educated about the psychological and other harms of using NPS and a culture of self-reporting of NPS use should be fostered in order to assist treatment
What’s next?
We know that NPS use is an issue that affects secure mental health units, both with regards to current use within the units and as a potential contributing factor for admission to the units.
Based on these findings, we recommend further research is prioritised in this area to determine the population wide impact of NPS induced mental illness.
In particular, we need a better understanding of the longer term impacts on mental health to inform effective interventions on prevention and management of clinical symptoms in mental health units.
Further information also needs to be provided about the acute psychological symptoms associated with NPS use.
Both for clinicians to ensure appropriate diagnosis and treatment and members of the public so that they are informed of the risks associated with NPS use.
Our review has also identified significant sociological impacts for people with mental health conditions relating to NPS within secure mental health units.
Units have also reported challenges in identifying those using NPS and tensions between users and non-users within the unit.
Issues have also been identified in relation to financial exploitation, allocation of leave, interference with treatment and safeguarding of vulnerable patients.
The findings from the evidence review also support that NPS use may have an impact on the physical health of those in secure mental health care.
To ensure health inequalities are reduced amongst those under the care of mental health services in England these findings clearly warrant further research. PHE, in partnership with NHS England, will be taking the case for further public health action on NPS forward.
We plan to hold an event to share the findings of this report and develop the necessary resources to support people with mental health conditions, and those involved in their care, affected by NPS.
Image: National Assembly for Wales

