
This week we publish our 5th update to “Routes to Diagnosis”, the foundation of England’s efforts to improve outcomes for patients diagnosed with cancer.
This publication is particularly relevant as we now have ten years’ worth of data to examine, covering over 3 million diagnoses of cancer.
What is Routes to Diagnosis?
The expert team within PHE’s National Cancer Registration and Analysis Service (NCRAS) link multiple routine datasets together to sequence patient events, working backwards in time from a cancer diagnosis.
We collate the results into eight different routes through which patients get diagnosed. We can then examine and compare the data by route, age, sex, ethnicity, deprivation, geographical area, and, crucially, patient outcome, that is the length of time they survive after being diagnosed.
It’s the biggest collection of data of this kind in the world, and by continuing to develop it we are building a unique insight to why some cancers in England are diagnosed later than others.
You can read more about the history and development of this work in one of my previous blogs: Big data in action: The story behind Routes to Diagnosis
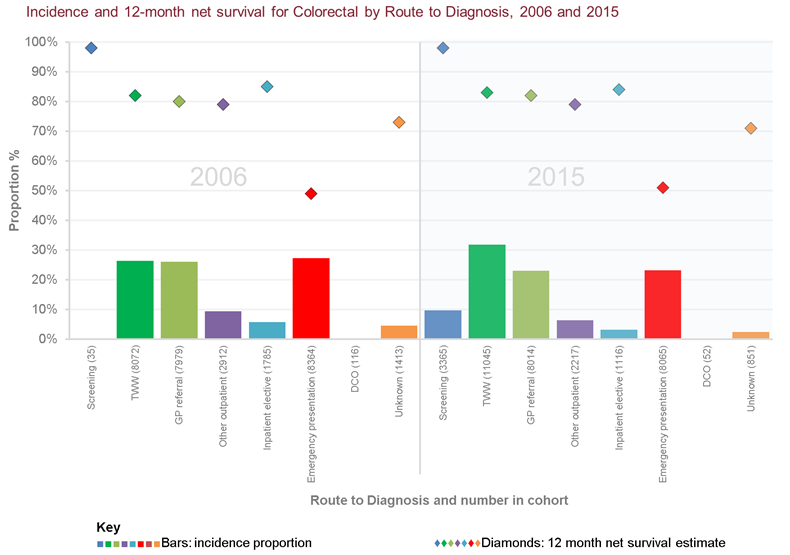
We know that some cancers and routes have much poorer outcomes than others. The proportion of cases diagnosed through the emergency presentation route varies from 1% for in-situ breast and in-situ cervical cancers to 65% for acute lymphoblastic leukaemia. However for every cancer type the survival rates are poorer for the emergency presentation route.
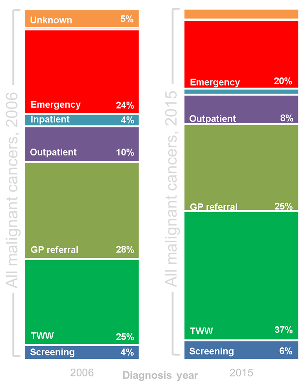
The data does show that there has been some change over time, like increased use of the Two Week Wait route (from 25% in 2006 to 37% in 2015, for all cancers combined), so we may be starting to see an improvement, as reported in some of our patient case studies.
GPs taking quick action
We hear many reports of GPs spotting cancer symptoms very quickly and referring patients rapidly through managed routes.
Barbara was diagnosed with bowel cancer following a referral to her GP from the blood transfusion service, after they refused a donation because she was severely anaemic. The GP immediately referred her using the Two Week Wait referral route and she had a colonoscopy in less than two weeks and surgery four weeks after that.
The cancer was late stage, and looking back Barbara can see that she had symptoms that could have suggested that something was wrong. “I thought that mine related to being overweight, sedentary and probably menopausal, so I didn’t see any point in going to the doctor. I didn’t know that anaemia was a symptom of cancer. I also thought that as I hadn’t had sudden, unexpected weight loss, then there couldn’t be anything seriously wrong.”
Barbara’s story highlights the role that public awareness campaigns, such as PHE’s Be Clear on Cancer, can play in alerting people to the signs and symptoms that might be caused by a developing cancer. We know that diagnosing a cancer earlier means more chance of being cured.
Emergency GP referrals
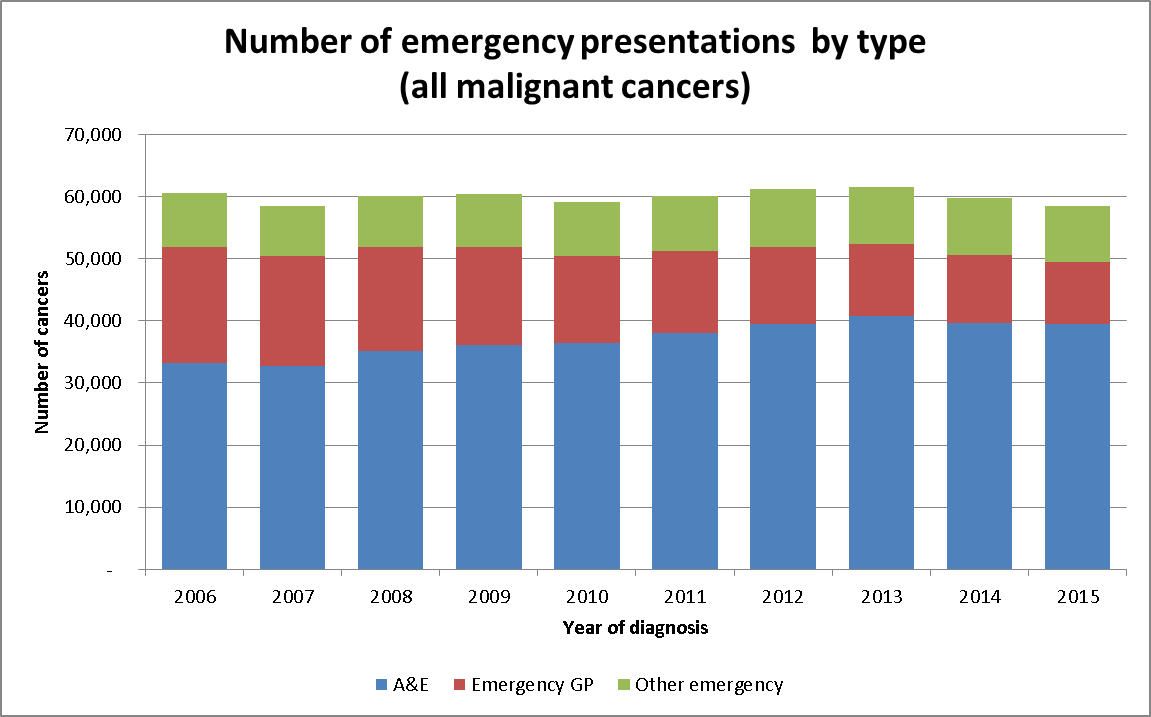
One aspect of the Routes to Diagnosis data that sometimes confuses people is that the emergency presentation route does not only refer to people going to A&E. GPs can also make emergency referrals direct to hospital.
The percentage of emergency presentations from GPs has decreased over time, for bowel cancer this has gone from 34% of emergencies in 2006 to 20% in 2015.
Overall, while the number of emergency presentations has gone down from 24% to 20% between 2006 and 2015, the actual number of people who are diagnosed through A&E has gone up over this time. Almost 40,000 cases of cancer a year are now identified this way.
This varies enormously by cancer type, and we are working in partnership with researchers at a number of universities to better understand which types of people are being diagnosed though this route.
Using data
This latest publication means that 10 years’ worth of data is now available for the NHS, the public, charities, policy makers and researchers to use to help improve early diagnosis and cancer outcomes.
The results show a continuing reduction in emergency presentations, however for most cancers the proportions diagnosed through this route are still high. Charities and patient groups have always been interested in the work, and people can directly relate the findings to their own experiences, as evidenced in the patient stories that we have included here.
There is also growing support from patients to use their data in research. For this blog I contacted patients through the ‘use my data’ community: use MY data is a movement of patients, carers and relatives.
They endeavour to highlight the many benefits that appropriate usage of healthcare data can make, to save lives and improve care for all.
"Data improves services and develops new treatments; data adds to knowledge and understanding; data saves lives." Patient Advocate, use MY data
Acknowledgements
Data for this project is based on patient-level information collected by the NHS, as part of the care and support of cancer patients. The data is collated, maintained and quality assured by the National Cancer Registration and Analysis Service, which is part of Public Health England.
The Routes to Diagnosis analytical work is led by Sam Winters, Senior Cancer Information Analyst, with support from many other colleagues in the team.

2 comments
Comment by Sandhya posted on
Very nice article, Thanks for providing the information. Good job. Keep sharing.
<a href="http://fightbonetumors.com/">Cancer Hospital in Hydera bad.</a>.
Comment by Sandhya posted on
Very nice article, Thanks for providing the information. Good job. Keep sharing.
http://fightbonetumors.com/