Dr Lauren Cowley, formerly a PhD student at PHE and now a postdoctoral researcher at the Harvard T.H. Chan School of Public Health, tells us about her time working on the front line in West Africa tackling the Ebola outbreak in Sierra Leone and Guinea. All photos were taken by Lauren in the locations she worked.
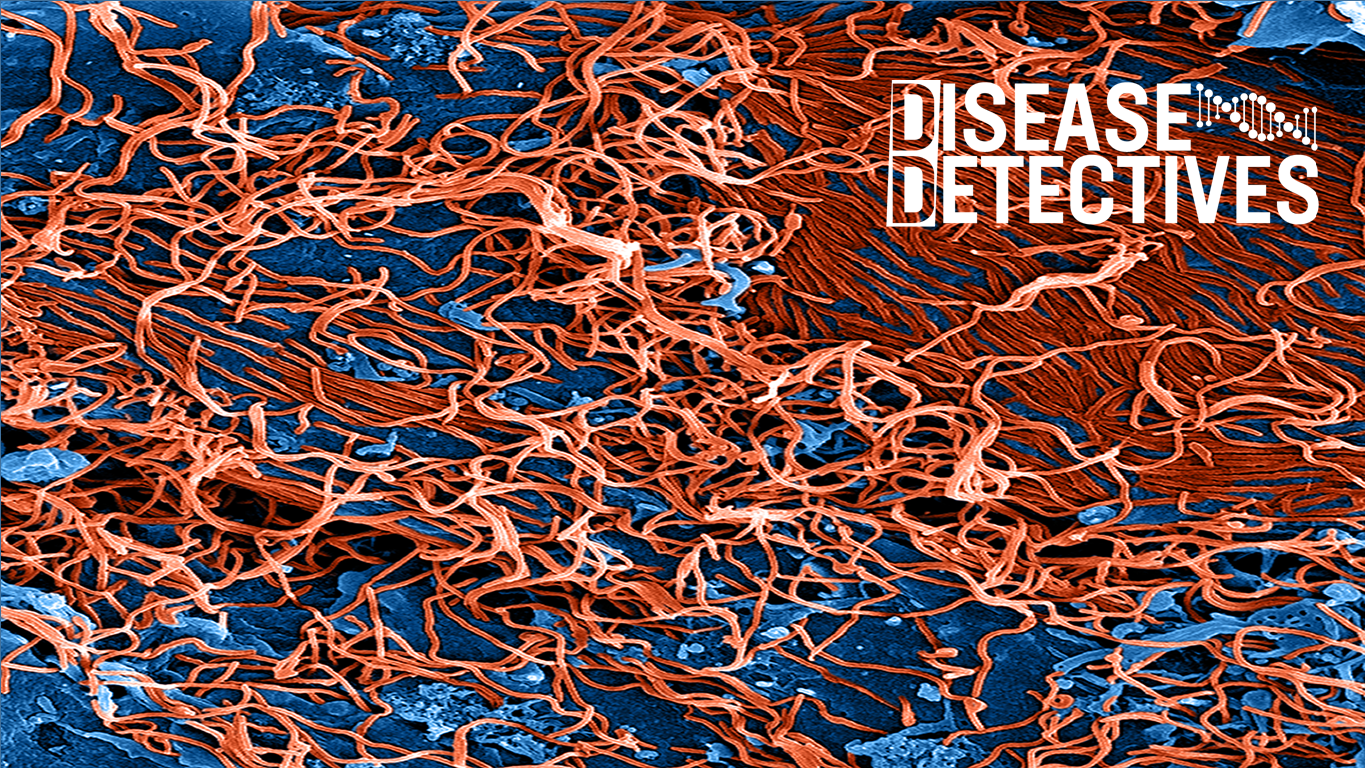
The news of the recent Ebola outbreak in the Democratic Republic of Congo brings back memories of the 2013-16 Ebola crisis in West Africa which was a shock to the whole world.
It highlighted the importance of investigating and responding to disease outbreaks before they become a global threat. The countries affected, namely Sierra Leone, Guinea and Liberia, suffered major loss of life with a very high case fatality rate, as well as damage to their economy and infrastructure.
During this time, I was in the same position as most – following the news and feeling helpless as I watched the tragedy unfold and worsen over time. Although I was a PhD Student at PHE at the time, the idea of being involved in tackling this outbreak did not cross my mind, let alone travelling to the affected countries to work in the field.
Soon this became a reality for me in November 2014, when I applied to be deployed to Sierra Leone. Suddenly, I was no longer just a spectator. I went from working on national diarrheal outbreaks in the UK, to working on the front line in Africa, responding to one of the biggest, most deadly, and most well-known disease outbreaks in modern day history.
My first deployment: Sierra Leone
In November 2014, I went to Sierra Leone for six weeks to work in the diagnostic laboratory, running blood, swab and urine samples to detect the presence of Ebola.
The symptoms of Ebola, especially at first, can be very generic as they include fever, diarrhoea and vomiting. As such, illness could often be mistakenly ascribed to other pathogens that are less life threatening. This can have major implications if the pathogen causing illness is, in fact, the Ebola virus.
This is why the diagnostic test was so important – it was the only way to categorically identify or exclude cases of Ebola. Diagnostic work is the first step that must be carried out to start and shape the process of case response and clinical management of the patient.

My second deployment: Guinea
My second deployment was to Guinea in June 2015 and was in collaboration with the European Mobile Laboratory and University of Birmingham to provide real-time sequencing of new Ebola cases.
This opportunity came about through social media. I had been in touch with contacts at the University of Birmingham (Nick Loman and Josh Quick) via Twitter, discussing my experiences during my first deployment. At the time, I was in the final year of my PhD, and was somewhat missing the excitement and sense of fulfilment from my first trip to West Africa. Therefore, when Miles Carroll, PHE’s Head of Research, contacted me to see if I would be interested in a real-time Ebola sequencing project, it was an immediate ‘yes’, and I was in Guinea within three weeks of receiving the first email about it.

Using Whole Genome Sequencing in the field
As the Ebola virus is spread through human-to-human transmission, Whole Genome Sequencing was an essential technique to use in surveillance and case response. The highly accurate technique allows the route of transmission to be traced throughout a country and beyond, characterises the infectious agent, and provides a high-resolution view of its evolution.
To find out more about the process of Whole Genome Sequencing, read our explainer blog here.
During the Ebola outbreak, a lack of local sequencing capacity and the difficulties of transporting samples to sequencing facilities far away meant that genomic surveillance was inconsistent. However, regular genomic surveillance is important, as the sequence data can be used to guide control measures, if it is generated quickly enough.
Before being deployed, the team I worked with devised a genomic surveillance system using a novel nanopore DNA sequencing instrument, which weighed less than 100 grams. A nanopore is a protein with a very small hole that allows DNA strands to be driven through it using an electric current. As each nucleotide passes through the pore, the current is affected and this change allows the sequence to be recorded.
All together, our system consisted of three of these instruments, four laptops, a thermocycler, a heat block, pipettes, and sufficient reagents and consumables. In April 2015, the team packed this into regular airline luggage and transported it to Guinea, where they started using the system for real-time genomic surveillance of the Ebola outbreak.

Components of the genomic surveillance system set up in the laboratory in Guinea
Once I joined the team in Guinea, I used the surveillance system to carry out real-time sequencing and analysis of all new Ebola cases for five weeks. We worked in partnership with local Guinean diagnostic laboratories to provide the sequencing results to the National Coordination in Guinea, which was provided by the World Health Organisation (WHO). We were able to generate results less than 24 hours after receiving a positive sample, and the sequencing process itself took as little as 15 to 60 minutes.
Setting up the laboratory
Our laboratory was a small, hut-like shipping container, which we set up at an Ebola treatment centre in what seemed like the middle of nowhere. Despite being in a treatment centre, we were not in danger of contracting the virus within our hut as we were in a ‘neutral zone of containment’, separate to where the patients were staying and the other side of all containment measures. This meant that the virus was contained and prevented, by several measures, from escaping into this zone.
It was completely safe to be handling the samples we were working with, meaning we did not have to wear personal protective equipment. We were only working with the raw extracted genetic material of the virus, and not all the viral machinery that is contained within the viral cell. The virus requires more than just its raw genetic material to effectively infect a human cell.

The shipping container laboratory in Guinea
Advanced technologies in resource-limited conditions
Working in resource-limited conditions and setting up our own laboratory meant that we faced inevitable obstacles along the way.
We encountered multiple logistical issues during our time in Guinea, with perhaps the most challenging being the lack of reliable, continuous power. This meant that we had to depend on unreliable electrical generators and uninterruptable power supplies that provide emergency battery power.
Further to this, internet connectivity was consistently poor, which particularly disrupted our ability to send data back to colleagues at the University of Birmingham for analysis. I often couldn’t access the sequencing software, and therefore had to send raw read files. Our Birmingham partners would then send back information about the relatedness of new cases to others already sequenced, and I worked closely with epidemiologists at the WHO to establish transmission chains.
Considering these challenges, I am proud of the work I did within this team, as I think we demonstrated the possibility of conducting such an advanced and impactful process in such resource-limited environments.
How I felt: The differences between the two trips
It goes without saying that it is nerve-racking to be deployed to a country where there is an active, deadly disease outbreak, causing loss of life at a rapid rate. Normally, you would avoid a place like this at all costs, so on my first trip I was cautious and naturally worried.
I felt more comfortable on my second deployment and I was able to enjoy the work I was doing more. Being the fastest sequencing conducted during a major outbreak to date, it felt like I was involved in something novel and important, particularly as it was influencing the scope of future work and decisions.
Despite the excitement of my role, the reality of the situation was that there was death, pain and social disarray all around us. The memory of seeing two doctors dressed in full protective suits feeding a dying 8-year-old girl fresh coconut water, after she had requested it as her last wish, will never leave me.
Everything about Ebola and the reasons behind why we were there is tragic, however being a part of the global effort to fight it was very rewarding and has taught me invaluable life lessons.
This programme of work was awarded the PHE Research Innovation Award in 2016. A current PhD student at PHE has recently returned from Nigeria, where she was a part of a team that successfully applied the same technology Lauren worked on to the Lassa fever outbreak.
Read more from Disease Detectives - keeping track of new and emerging infectious diseases.
