
Most of us want to live in good health for as long as possible; but while people are generally living longer, outcomes still vary hugely across the country as disturbing inequalities persist.
For example, we know that in the most affluent areas people enjoy 19 more years in good health than those in the poorest areas: the opportunity to be healthy appears to be very different depending on where you live.
As the NHS takes a hard look at its finances, it is significant that the poor health experienced by the poorest communities costs the NHS an extra £4.8bn a year. Harm to the economy in general through productivity losses is even greater at over £30 billion per year.
A big part of our role at PHE is to provide the best evidence and data to guide action to improve and protect health. We are proud to have been centrally involved in a new analysis of the Global Burden of Disease study, published today in The Lancet.
The work is a partnership between PHE, the University of Washington, the University of East Anglia and many colleagues in leading universities and organisations across the UK.
This study is incredibly timely, providing a detailed and comprehensive picture of the health of people in the UK just at the time when it can be used to shape the forthcoming NHS long term plan.
The extra investment in the NHS will not be followed by improvements in health unless those extra resources are directed to the areas of greatest need and opportunity – that’s what this paper allows.
It provides data on mortality, illness and disability burden, as well as the risk factors linked to burden from 1990 to 2016. Results are available for 150 Counties and Unitary Authorities in England, and for Scotland, Northern Ireland and Wales, to aid local and national policymakers to prioritise efforts to prevent ill health, not just deal with the consequences.
By comparing estimates for local authorities according to levels of deprivation the report emphasises the importance of addressing the wider determinants of health.
Premature deaths and burden of disease
The most common causes of premature death in 2016 are similar in all four UK counties: heart disease; lung cancer; stroke; chronic obstructive pulmonary disease (COPD); and dementia.
Interestingly, more affluent local authority areas appear to have experienced greater improvements in mortality before 2000, but this changed after 2010 when the national slowdown was more noticeable in relatively affluent areas (at least for the particular measures used in the GBD study).
A striking finding from the report is that on a day-to-day basis, the most common causes of burden for people are back pain, poor mental health, skin conditions and sight and hearing loss.
These problems tend to attract less attention than causes of early death such as heart disease and cancer, but together they account for a huge amount of ill health and of course place a massive burden on the NHS and other care services.
Unhealthy lifestyles
This data demonstrates exactly where the big opportunities are for the NHS as it works to develop its long term plan – prioritising the prevention of harm from smoking, cardiovascular disease (CVD) and obesity, which you can read about in our previous blog.
In all four countries, more than half of premature deaths are associated with potentially preventable risk factors including tobacco; unhealthy diets; obesity; alcohol and drug use; low physical activity; and environmental factors, such as air pollution.
The contributions of the ten leading risk factors to years of life lost were similar across the countries in UK, but with higher percentages (population attributable fractions) attributed to tobacco use in Scotland, and of alcohol and drug use in Scotland and Northern Ireland.
Since 2010, the annual rate of reduction in premature deaths linked to most major risk factors has slowed – leading to a slow-down in the rate of increase in life expectancy – apart from alcohol where the situation has remained roughly unchanged since 2000.
Cardiovascular disease remains the leading cause of mortality suggesting renewed and sustained effort is required to reduce risk factors such as high body mass index, high fasting glucose, high blood pressure and high cholesterol (all ranked in the top 10 risk factors in the UK).
PHE’s Health Economics team has published a series of Return on Investment tools to support commissioners in planning effective prevention.
Our latest tool helps commissioners decide the best approaches to preventing cardiovascular disease by showing the predicted cost and health benefits of different approaches to tackling major risk factors such as high blood pressure and high cholesterol.
Regional inequalities
The north of England generally suffers much poorer health than the rest of England, with lower life expectancy and earlier onset of chronic illness and disability.
This geographical effect is however largely driven by the stark division in health between rich and poor areas in every region in the country. On average, poorer groups die earlier and get sicker quicker.
The underlying causes of both geographic and socio-economic health divides are in large part the same: differences in poverty, power and resources needed for health.
There are however some geographical anomalies. Some London Boroughs and Birmingham have relatively low levels of risk and premature mortality compared with similarly deprived parts of Liverpool and Manchester. This suggests the need for specific action to respond to the challenges facing these northern cities beyond any nationally constructed intervention.
One explanation may be that London Boroughs have relatively low levels of certain key risk-factor exposures, particularly tobacco and dietary risks.
Other possible factors may be better educational performance of children from poorer communities in London; selective movement of less healthy people out of London; more movement of less healthy people out of London; and healthy younger migrants moving in.
Access to health services may also be a factor, with some evidence suggesting that health services in London are relatively better funded compared to the North East and North West of England.
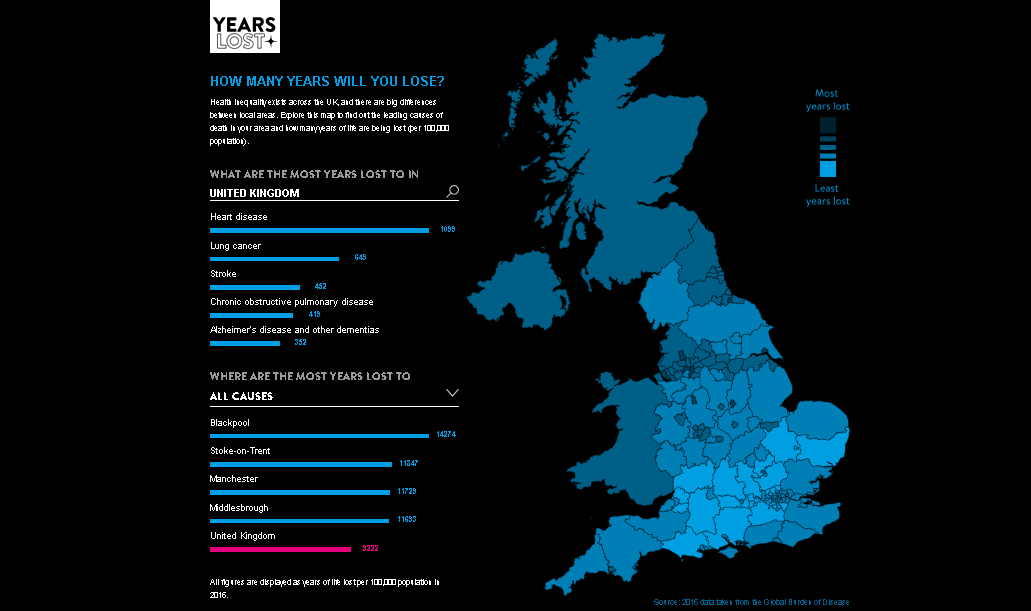
The University of East Anglia has created an interactive map which allows users to explore the data and learn how many years of life are lost to the UK's leading 20 causes of death for people in their area.
So what can the NHS do?
The rapidly changing epidemiology presents a challenge to which the NHS must respond. There is a need to focus on preventing as well as treating the conditions causing the greatest disease burden and the greatest demand for our health and care services.
Now in its 70th year, those demands on the NHS have changed significantly even in the last decade – we need to adapt fast and prioritise efforts to prevent ill health as a nation, and not just deal with the consequences.
We want this report to be used as a reference point for policymakers as they think about the full range of policies across government that have an impact on health.
The opportunity to enjoy good health is a fundamental human right. The aim of securing health for all regardless of background is at the heart of the NHS and one reason we are so proud of it.
But just providing treatment free at the point of care is not enough – it is time to give everyone an equal opportunity to lead a healthy life, and seek to achieve a fairer, healthier and more prosperous future for everyone in England.
You can read the full analysis via The Lancet.
