
The latest edition of Health Matters, PHE’s professional resource, focuses on smoking among the population of people living with a broad range of mental health conditions, ranging from low mood and common conditions such as depression and anxiety, to more severe conditions such as schizophrenia and bipolar disorder.
This blog provides a summary of the full edition’s content.
The scale of the problem
Smoking rates are declining in England, with prevalence in adults (aged 18+) having decreased from 17.1% in 2013/14 to 14.5% in 2018/19 (General Practice Patient Survey data).
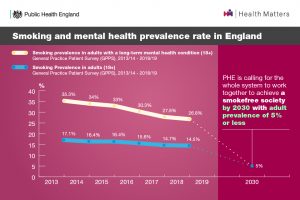
While a decrease in smoking rates has also been seen among adults with a long-term mental health condition – falling from 35.3% in 2013/14 to 26.8% in 2018/19 – prevalence remains substantially higher, despite the same levels of motivation to quit.
PHE’s Local Tobacco Control Profiles for England show that as the severity of mental health conditions increases, smoking prevalence is higher.
In 2014/15, prevalence in all adults (aged 18+) was 16.4% and prevalence in adults living with:
- anxiety or depression was 28.0%
- a long-term mental health condition was 34.0%
- serious mental illness was 40.5%
Even common mental health conditions, such as anxiety and depression, are associated with a greater likelihood of smoking and of being highly dependent.
People with poor mental health die on average 10 to 20 years earlier than the general population, and smoking is the biggest cause of this life expectancy gap. A joint study by the Royal College of Physicians and Royal College of Psychiatrists found that a third of cigarettes smoked in England are smoked by people with a mental health condition.

The benefits of quitting smoking for mental health
Addressing higher dependence on tobacco is likely to support smoking cessation, and in turn, reduce health disparities. For people with a mental health condition, smoking cessation improves both physical and mental health and reduces the risk of premature death. Stopping smoking can even be as effective as antidepressants.
The smoking cessation intervention for severe mental illness (SCIMITAR+) trial found that quit support is effective in this population. The incidence of quitting at 6 months shows that cessation can be achieved, but the waning of this effect by 12 months means more effort is needed for sustained quitting.
Smokers reporting depression or anxiety are more likely to be offered stop smoking support by their GPs, but this does not always translate into quitting as higher nicotine dependence is seen amongst this group. When used with stop smoking treatments, e-cigarettes can help people living with a mental health condition to quit.
Smokefree mental health trusts
In 2016, NHS England’s Five Year Forward View for Mental Health recommended that all inpatient mental health services should be smokefree in 2018. The government’s Tobacco Control Plan for England then set out a commitment to implement comprehensive smokefree policies, including integrated tobacco dependence treatment pathways, in all mental health services by 2018.
There are 3 things that make a trust smokefree:
- every frontline professional discussing smoking with their patients
- stop smoking support offered on site or referral to local services
- no smoking anywhere in buildings or grounds
1 in 5 mental health trusts still do not have a comprehensive smokefree policy in place and the most commonly identified barriers to its implementation are:
- staff resistance
- patient resistance
- insufficient resources
- lack of senior management leadership

This edition of Health Matters details where progress is still required to make all mental health trusts in England smokefree. It also covers where additional action must be taken to ensure community mental health staff are equipped with the appropriate training and expertise they need to deliver very brief advice (VBA) and prescribe stop smoking medicines.
Call to action
The government’s recent Prevention Green Paper highlights that smoking rates remain stubbornly high among people living with mental health conditions. It acknowledges that tackling this inequality is the core challenge in the years ahead and that if England is to achieve being a smokefree society by 2030, bold action is required to both discourage people from starting in the first place and support smokers to quit.
All mental health practitioners should support quitting smoking routinely as part of mental health care to improve physical and mental health outcomes. This must involve:
- asking all patients if they smoke and recording the data
- using tobacco dependence treatment pathways for support

There must also be better use of both stop smoking medicines and e-cigarettes, particularly in community mental health services where most people with mental health conditions come into contact with their care provider. Mental health services, local authorities, commissioners, and care quality commission (CQC) inspectors all have a role to play.
Visit the Health Matters area of GOV.UK or sign up to receive the latest updates through our e-bulletin. If you found this blog helpful, you can read other Health Matters blogs here.
