
Setting the foundations for health and wellbeing during pregnancy and in the early years is crucial to ensure we give every child the very best start in life as possible.
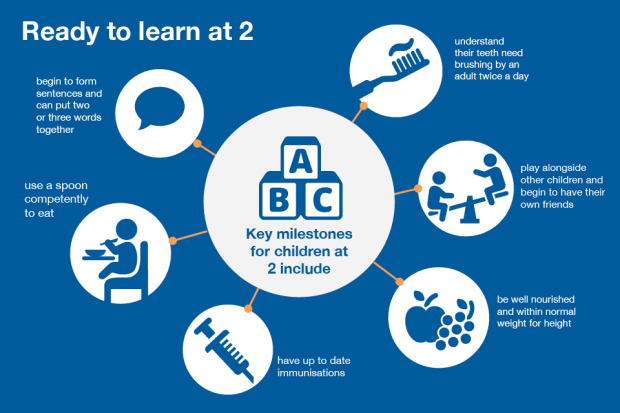
It is also important that support and access to effective interventions is continued throughout the school-aged years. New parents need to be supported as they make the transition to parenthood and have access to support when they need it most. This will help ensure their child can thrive and achieve - we want all children to be ready to learn at 2, ready for school at 5 and ready for life when they reach adulthood.
The Healthy Child Programme, launched 11 years ago, is still the national evidence based universal programme for children aged 0-19. The programme provides the bedrock for health improvement, public health and supporting families.
There is national commitment to modernise the programme over the next few years, to ensure the programme is both current in terms of evidence and context. The NHS Long Term Plan and the growing movement around place-based approaches provides impetus for the modernisation. Providers will be equipped to design effective, family-oriented services - with children at the heart of how it is structured and functions - that build on local assets and community-based approaches with a stronger emphasis on what works.
Impact of COVID-19
The updated Healthy Child Programme will also need to consider the challenges and impact of COVID-19. No Child Left Behind clearly highlights the need for a focus on reducing vulnerabilities and addressing inequalities, together with a comprehensive approach to identifying and addressing the needs of children and families.
The care delivered by health visitor and school nurse teams and their community nurse colleagues has been and will continue to be an essential part of the response to and recovery from the pandemic, supporting families and communities through indirect impacts and ‘hidden harms’ especially in deprived communities and among the most vulnerable. The updated programme is timely as the public health nursing system endeavours to restart its work with the most vulnerable families.
Preconceptual care and extending to 24 years for the most vulnerable
As part of the modernisation we have committed to extending the programme to include preconceptual care and to extend from 19 to 24 years of age – for those children with a statutory requirement. This includes some of our most vulnerable children, for example those in the care system and with additional health needs or a disability.
Modernising the Healthy Child Programme will take time; new evidence and policy direction will need to be included, together with co-production and engagement with professionals, children, young people and families.
Over the last year we have been reviewing the evidence and intervention schedule which underpin the programme. The modernisation will also include developing suites of resources to address key priority areas, for example, preconceptual care, maternity, effective care continuity between midwifery and health visiting, and narrowing the word gap (speech and language skills) to address inequalities. These resources are designed to support local delivery and commissioning and include:
- evidence-based resources, aimed at health and social care providers as well as service users, to help women with severe mental illness access preconception care and advice
- High Impact Areas for maternity
- an interactive Healthy Pregnancy Pathway
- material to help local areas improve levels of speech, language and communication in the early years in children, and identify those with additional needs earlier.
The Healthy Child Programme is led by health visitors and school nurses, who work in partnership with a range of professionals and agencies to support children and families. Today we are publishing the revised health visiting and school nursing model, which replaces the “456” model, to focus further on needs assessment so that interventions are personalised to respond to children and families’ needs across time.
The new model aims to capture the full extent of both the health visitor and school nurse offer – as many local services were offering so much more than the ‘5’ contacts, it was therefore important to ensure this was clearly articulated. The model suggests opportunities for further contacts or opportunities to provide support; for example, within early years contacts at three and six months, to support breastfeeding, mental health, healthy diet and safer sleep. Clearly, health visitors will use their professional and clinical judgement to determine if the contacts are required and what approach would work with the family.
The revised model, commissioning guidance and high impact areas have been updated with new evidence and emerging policy developments, based on feedback from service users, professionals working in this space and commissioners. We will continue to review these publications as part of further work on the modernisation of the Healthy Child Programme.
Parent-facing digital content
The refreshed programme will also include parent facing digital content, enabling parents and carers to be full and active partners in their children’s health, and as young people grow in agency, they will be equipped with the knowledge and information to take individual health responsibility.
The production of all the resources underpins the modernisation of the Heathy Child Programme, which will take a further 2-3 years and this is important to ensure we have a robust, universal evidence-based programme which can support the health and wellbeing of our children and young people for future generations.
