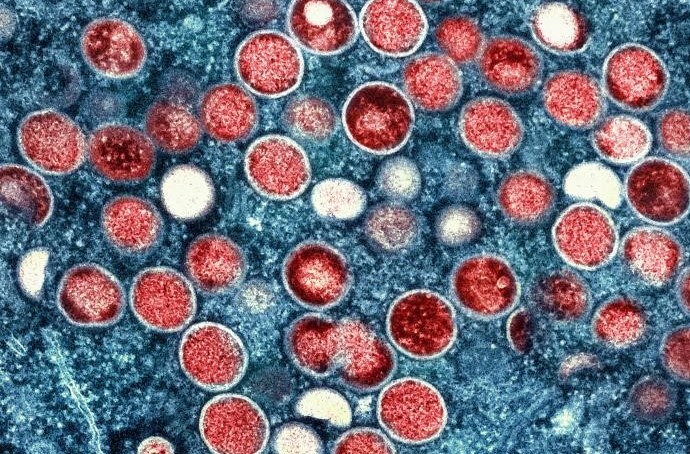
Credit: CDC/ National Institute of Allergy and Infectious Diseases (NIAID)
This blog post was reviewed and updated in April 2025.
The World Health Organization (WHO) declared a public health emergency of international concern because of the rapid spread of a mpox virus strain, clade I, after its emergence in the Democratic Republic of the Congo (DRC) last year, and the potential for the virus to spread further across countries in Africa and outside the continent.
As of March 2025, clade Ia and Ib mpox are no longer classified as a high consequence infectious disease (HCID).
The UK Health Security Agency (UKHSA) works with the NHS, local authorities, and other government departments to ensure we are ready to respond to any cases we see in the UK and help prevent transmission.
In this blog post, we share more information about what mpox is, the different clades, the key symptoms and how UKHSA works with partners to monitor and respond to any cases
What is mpox?
Mpox (formerly known as monkeypox) is a viral infection that spreads through close person-to-person contact. Like many diseases caused by a virus, mpox has different types or ‘clades’. There are two major clades of mpox, known as clade I and clade II.
Clade II mpox has been present in the UK since 2022. Clade I mpox has previously only been reported in 5 countries in Central Africa but there is now increasing transmission of Clade I mpox in several countries in East and Central Africa. Cases have also been reported in countries outside of the African continent with a small number detected in the UK.
Anyone can catch either clade of mpox, as it spreads from person-to-person, through close contact (including intimate or sexual contact) with someone who has symptoms of mpox, through contact with contaminated materials, such as bed sheets or towels, and contact with infected animals.
Mpox does not spread easily between people unless there is close contact with someone who has symptoms.
Spread between people may occur through:
- direct contact with rash, skin lesions or scabs (including during sexual contact, kissing, cuddling or other skin-to-skin contact)
- contact with bodily fluids such as saliva, snot or mucous
- contact with clothing or linens (such as bedding or towels) or other objects and surfaces used by someone with mpox
It is possible that clade I mpox may spread between people through close and prolonged face-to-face contact such as talking, breathing, coughing, or sneezing close to one another. However, there is currently limited evidence so this will be updated as new information is available.
Spread of mpox may also occur when a person comes into close contact with an infected animal (rodents are believed to be the primary animal reservoir for transmission to humans), or materials contaminated with the virus. Mpox has not been detected in animals in the UK.
What are the symptoms?
The symptoms of mpox include:
- A skin rash with blisters, spots or ulcers that can appear anywhere on your body (including your genitals)
- Fever
- Headaches, backache, and muscle aches
- Joint pains
- Swollen glands
- Shivering (chills) and exhaustion
A rash usually appears 1 to 5 days after a fever, headache and other symptoms. The rash (spots, blisters or ulcers) often begins on the face, then spreads to other parts of the body. This can include the mouth, genitals and anus. The number of sores can range from one to several thousand.
If you have recently travelled to any of the affected countries, and have any new spots, blisters or ulcers that have developed within 21 days of returning, please isolate at home and call NHS 111 for advice, letting them know your travel history.

What is the treatment for clade I mpox?
The symptoms of mpox can range from a few spots to a severe rash and illness. Treatment will depend upon the needs of the individual patient but may include admission to a specialist hospital.
New-born babies, children, people who are pregnant and people with underlying immune deficiencies may be at higher risk of more serious mpox disease and death.
UKHSA is working closely with the NHS and academic partners to determine the characteristics of the pathogen and further assess the risk to human health.
Is mpox clade I in the UK?
A small number of imported clade I mpox cases have been confirmed in the UK to date, however the wider risk to the UK population remains low.
Clade I mpox was detected by UKHSA using polymerase chain reaction (PCR) testing.
Preparations to detect cases of mpox have included extensive monitoring and surveillance of international cases, ensuring rapid testing for all mpox strains is available, equipping healthcare professionals with guidance and advice on how to respond to potential cases, reducing the risk of transmission and close working with international partners to make sure our plans are informed by the latest global picture.
In 2022-23, there was a global outbreak of clade II mpox, including in the UK, which appears to be a less severe strain. This was primarily driven through sexual contact. Clade II mpox cases are still present in the UK.
What is the risk to the public’s health?
The overall risk to the wider public is currently considered low. However, due to the severity of clade I mpox we are reminding people who have recently travelled to the affected areas to be aware of signs and symptoms and contact a healthcare professional if they are concerned.
What is the travel advice?
Currently, the risk to most travellers is low and vaccination against mpox infection is not recommended for the majority of people.
Those travelling to areas affected by the ongoing outbreak should take sensible precautions to protect themselves from the risk of infection by reducing touch or sexual contact, especially with individuals with a rash.
You can see a list of countries where cases of mpox clade I have been reported on the Travel Health Pro website. We recommend that anyone planning to affected countries check the latest travel advice published by the FCDO.
People who are travelling to affected countries can seek health advice from their GP or from a travel health clinic.
Who is eligible for the vaccine?
The vaccine will be offered to those eligible in stages as it becomes available over time and based on clinical need.
The government has agreed that the following groups should be offered vaccination, based on expert advice:
- gay, bisexual, or other men who have sex with men (GBMSM) previously identified at higher risk of coming into contact with mpox as a continuation of the clade II mpox vaccination programme, as advised by the Joint Committee on Vaccination and Immunisation (JCVI) in November 2023 – planning is under way for how and when the vaccine will be rolled out as part of this existing programme
- certain healthcare workers in agreed infectious diseases inpatient units and sexual health services
- certain specialist healthcare and humanitarian workers who go to affected countries to work within mpox response or sites with active outbreaks following a risk assessment
- close contacts of a confirmed case to lower their risk of becoming infected and reducing their risk of severe disease
Is the vaccine effective?
UK and global evidence from the mpox clade II outbreak in 2022-23 suggests that the currently available vaccine is effective if given to individuals before they are exposed to the infection (approximately 70% to 85%, with the majority of the protection provided by the first dose) with more limited protection if given after exposure (~20% effective). The vaccine is expected to work as well for clade I mpox as for clade II.
How can we protect ourselves and others?
Anyone can catch mpox, so if you have recently travelled to an affected country, be aware of the symptoms. If you think you might have the infection, avoid close contact with other people, self-isolate at home and speak to a healthcare professional as soon as possible.
Additional resources
If would like to find out more about this mpox outbreak, the following links contain lots of helpful information and updates:
