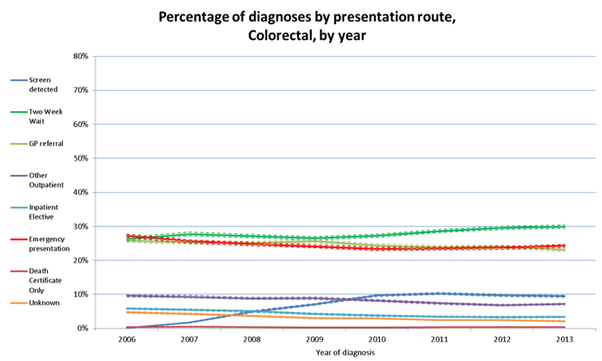
Today we published new data showing the different diagnosis routes for people with cancer. We have used the latest available data to produce an extensive set of results for over 2 million patients diagnosed with cancer between 2006 and 2013.
The headline figures are encouraging: the proportion of cancers diagnosed through an emergency route has decreased from 24% to 20%, whilst the proportion of cancers diagnosed through urgent GP referral with a suspicion of cancer, the Two Week Wait route, has increased from 25% to 34%.
The latest figures also clearly show the impact of the roll out and age extension of the bowel cancer screening programme.
Routes to Diagnosis is a great success story for PHE’s National Cancer Intelligence Network (NCIN). These updated results have been eagerly awaited by many of our partner organisations and stakeholders, not least the cancer charities and patient groups.
Previous results have been quoted by ministers, chief executives, campaigners and other influential leaders across the country, if not the world.
The story behind this project is one of collaboration and innovation. Conceived back in 2009, when NCIN was a young network, the seeds were sown when Cancer Research UK pushed us to quantify how people come to be diagnosed with cancer.
We knew that survival rates for cancer in England and the UK were poor compared to our European counterparts and suspected it might be due to later diagnosis.
At that time we knew that less than 10% of cancers were diagnosed through screening, and understood something about the percentage of people being referred as a Two Week Wait, but we had no idea how many came via other GP referrals, or through A&E, or were picked up in secondary care, say when a patient is being treated for an unrelated condition.
The suspicion was that a significant amount of late cancer diagnoses arise in these cases where patients have not gone through screening or the urgent referral route.
I remember somebody speculating at the time that we may find out that as many people are diagnosed through going to A&E as are diagnosed through all our current screening programmes put together - quite a sobering thought.
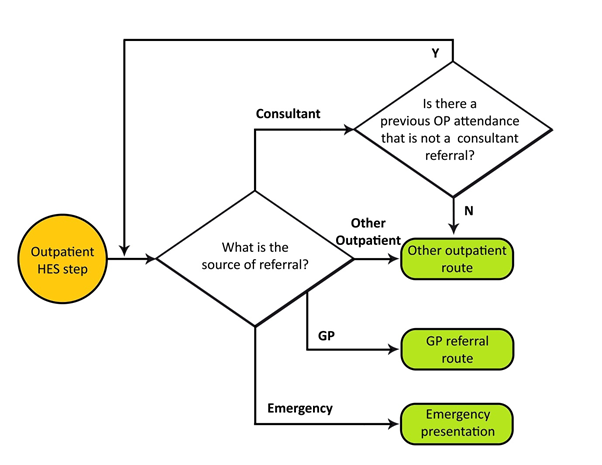
The challenge was to use routine datasets and consider how we could mesh together a variety of data sources, using some clever algorithms to sequence patient events working backwards in time from a cancer diagnosis.
Then after the data had been meshed & sequenced the results could be scrutinised by route, age, sex, ethnicity, deprivation and geographical area. Crucially, the patient outcomes, namely survival time after diagnosis, could be examined and compared.
The original concept was developed in close partnership with Brian Cottier, a true visionary and big data maverick in the cancer intelligence field.
His early death in 2009 necessitated a re-think to the project approach, but all was not lost. Under the leadership of Chris Carrigan, Head of the NCIN, local Cancer Network, regional Cancer Registry and national Cancer Action Team colleagues worked together across traditional organisational boundaries to define and test the complex algorithms that describe the many different pathways taken by patients to their cancer diagnosis.
The project team identified 135 different pathways to diagnosis. These were grouped into the eight Route categories that we are still using today. In early 2010 we tested the emerging results, based on patients diagnosed in the South West in 2007 (just under 60,000 cases), with Professor Willie Hamilton, a highly respected figure in the world of primary care diagnostics.
Willie had undertaken small scale studies on this topic in the past and so we were reassured by his assessment that the results looked pretty much as expected and that we must be doing something right.
During 2010 the results were reviewed and tested and the project up-scaled to cover all patients diagnosed in England in 2007. Professor Sir Mike Richards, then the Cancer Tsar, provided crucial clinical interpretation and leadership throughout the development of the work.
Initial results were presented at the NCIN annual conference in June 2010 and then published later that year. It would be fair to say that the headline figure showing that almost a quarter of patients were diagnosed after an emergency presentation was unexpected and shocking: the front page of the Daily Telegraph said it all:
1 in 4 cancers diagnosed late - patients are diagnosed only after being taken to hospital in an emergency, says study
The methodology was published in the British Journal of Cancer in 2012, and the results have been expanded and updated a number of times since the original briefings.
In big data terms, over 118 million records were used to generate the results that we are publishing today.
The project team has also grown and more people than ever before now work tirelessly behind the scenes to produce quality assured briefings and workbooks like those that we are publishing today.
Our motivation lies within the rich detail that the results are able to give us, and in the variation and inequalities that our data continue to reveal. When we look behind the averages we are confronted with stark realities, for example:
- 50% of pancreatic cancer patients present through an emergency route, with only 10% of those people surviving a year after diagnosis.
- For women diagnosed with ovarian cancer, 20% of those under 50 are diagnosed as an emergency, compared to 51% of those aged over 85.
- For people with colorectal cancers, only 7% in the most deprived areas are diagnosed through screening compared to 11% in the least deprived areas.
Too many people with cancer are still being diagnosed too late. We have a responsibility to utilise the cancer data that we are entrusted with to ensure that we are doing all that we can to help understand why this is and what can be done to make a difference to patients.
Routes to Diagnosis is one small but significant part of this endeavour, and one that I am immensely proud to have been involved in for the last six years.

1 comment
Comment by Rebecca Rennison (Target Ovarian Cancer) posted on
The Routes to Diagnosis data shows that of those women diagnosed with ovarian cancer following an emergency presentation, less than half live for a year or more following diagnosis, compared to 80 per cent of those women diagnosed following a referral from their GP. The data also tells us that more and more women are being diagnosed earlier; while almost one in three women with ovarian cancer were diagnosed following an emergency admission in 2006, just over one in four were diagnosed via this route in 2013. This helps show the impact that work to improve early diagnosis is having and the Routes to Diagnosis data helps us track these changes and continue to work to ensure more women are diagnosed early.