Antimicrobial resistance (AMR) occurs when organisms that cause infection, like bacteria, develop resistance to medicines like antibiotics. The World Health Organization estimates that there are 4.95 million deaths per year associated with AMR and the issue is a top public health priority for policymakers in the UK and around the world.
In December 2017, Public Health England set about raising public awareness and understanding of AMR to tackle the incorrect use of antibiotics by the general public and healthcare professionals.
Over a three-year period, the Keep Antibiotics Working campaign was targeted at groups who were most likely to use antibiotics (mothers of children aged 0 to 16, and people aged over 50), and healthcare professionals dealing with patient care and prescribing.
In a peer-reviewed study investigating the impact of the campaign, we found it reached the target audience, boosted awareness, and supported GPs, as well as increasing knowledge, changing attitudes, and increasing concern about AMR.
Dancing pills
The campaign was fronted by a group of singing and dancing anthropomorphic antibiotic pills, who serenaded our audiences with a fun, catchy and engaging song about the importance of only taking antibiotics when you need them and following your healthcare professional’s advice.
This was run in advertising across television and video-on-demand, radio, newspapers, billboards and other outdoor displays, and on social media.
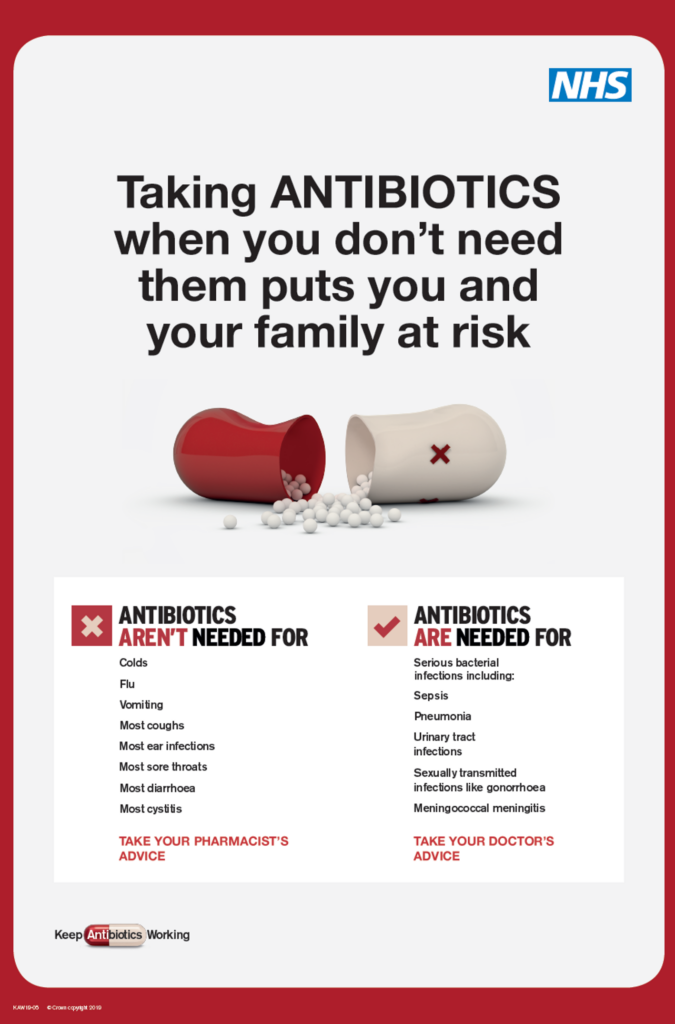
The campaign also included patient resources like information leaflets and posters for healthcare professionals to give to members of the public.
Investigating impact
In November 2023, UKHSA published a study in the academic journal Eurosurveillance evaluating the impact of the campaign.
We wanted to find out whether we had been successful in reaching the general public and our specific target audiences, and if the public’s knowledge, awareness and understanding of antimicrobial resistance improved due to the campaign.
We also wanted to investigate whether correct antibiotic usage increased, if GPs were more confident to decline antibiotics, and if demand from patients went down.
How was the study undertaken?
We collected questionnaire data from the public before and after each campaign burst, which ran for three months each year.
Our target sample size was 1,000 respondents for each questionnaire wave. Samples were then increased with each wave through targeted sampling among key groups, such as mothers of children aged 0 to 16.
The public sample was weighted to ensure it was nationally representative by age, gender, region, and socioeconomic status.
What we found
Over the three years of activity, we saw increases across key metrics. This included a significant jump in awareness across target audiences, with a 20% increase among mothers of children aged 0 to 16.
- Among our target audiences, we saw a 16.7% increase in awareness and understanding that “antibiotics will stop working for you if taken incorrectly”, as well as a 7.5% increase in awareness and understanding that “taking antibiotics unnecessarily puts you and your family at risk”.
- There was a reported increase in appropriate antibiotics usage, too. The number of respondents in our target audiences who reported that they were unlikely to request antibiotics for themselves or their child increased by 6.85% and 18.5% respectively following the first year that the campaign was run.
- Respondents also reported feeling more concerned about AMR, both in relation to themselves (significant increase of 28%) and those within their care (significant increase of 11% from 54% to 60%).
- GPs felt the campaign supported them to say no to patients requesting antibiotics (> 89%), where not clinically appropriate. From pre to post 2017, GPs who were aware of the campaign were significantly more confident to refuse prescribing antibiotics. In 2018, GP’s who were aware of the campaign were more likely to explain the inappropriateness of using antibiotics to treat viral infections to patients.
What do these findings tell us?
These findings clearly demonstrate the important role that communication campaigns can have in raising awareness about serious public health concerns like AMR.
Although Keep Antibiotics Working is no longer a live media campaign, the digital resources are still available and have been translated into 12 additional languages. We have also continued to engage the public through other tools, including:
- Antibiotic Guardian: a campaign devised to follow up on the awareness raised by Keep Antibiotics Working with a powerful engagement activity. To date, more than 205,000 pledges have been made from individuals across more than 120 countries about how they plan to make better use of antibiotics and contribute to tackling AMR.
- The e-bug Programme: an initiative seeking to reach and equip those who work with, or support children and young people (aged 3 to 25 years) in all communities with information and activities to build knowledge around microbes, disease, hygiene, vaccination and AMR.
- TARGET Antibiotic Toolkit: a toolkit designed to support primary care clinicians to champion and implement antimicrobial stewardship activities.
- World AMR Awareness Week toolkit: a toolkit which aims to provide quick and ready-to-use material to support your WAAW campaigns. The toolkit is focused on digital messaging to support speed and ease of communication while including a wide variety of suggestions for engagement with different groups of people.